Surgery is usually the first thing people think of when they want to deal with colorectal cancer. However, did you know that there are many other treatments and tests that you can choose from?
To avoid mistakes on which one tests and treatments to choose, let me, Dr Ng Chee Yung, give you the guide on how to choose the right colorectal surgeon.
What is a colorectal surgeon?
As a colorectal surgeon (colon and rectal surgeon), I am a physician who specialises in the medical and surgical treatment of conditions that affect the lower digestive tract.
I went through extensive education and advanced training. I have comprehensive knowledge about general surgery and in the diagnosis and treatment of disorders of the colon, rectum, and anus.
What special training do you go through to be a colorectal surgeon? Is there a special certification?
Colon and rectal surgery is a surgical speciality. I graduated from a 4-year undergraduate program and successfully completed an accredited 4-year medical program. After that, I entered a general surgery residency involving 5 to 6 years of extensive training.
After completing my surgical residency, I did an additional 1 to 2 years of training to specialise in colon and rectal surgery. I had a minimum of 14 years of education and training before I applied for board certification.
What are some common cases you see in your practice?

The most common type of cancer affecting Singaporeans is colorectal cancer. We know the cycle of turning colon cells into polyps, and then colorectal cancer, very well.
There are many types of cases I have encountered in my practice. Some cases referred to me include:
- Haemorrhoids
- Tummy pain
- Or screening for colorectal cancer
To sum it up, I have seen many secondary referrals from other doctors that have diagnosed these colorectal conditions.
What is the most interesting case you’ve seen in your practice?
Some of my cases tend to be complicated. For example, a man who had prostate cancer was misdiagnosed with rectal cancer. He was also advised by other doctors that his case might not be suitable for any type of or surgery.
However, since the rectum is close to the prostate, the doctors improvised and the surgery turned out well, and he is currently doing fine.
What is the patient journey like?

First, you come and register with me. You might have been referred to me by friends, family, or some other recommendation. This is followed by a quick health screening in the form of a questionnaire and finished with a consultation where we will do some physical examinations and make a diagnosis.
Second, we will plan a treatment. Many patients require some type of procedure, most commonly an Endoscopy or a Colonoscopy. In addition to that, we will brief the patient on what to expect. You have to be counselled on how to prepare and what to expect on the day of the procedure. The procedure is usually quick and seamless.
Related: How is colon surgery performed?
Finally, in cases where the procedure went well, we will plan a follow-up appointment with you and run through any test results that are still pending and go through the results of the procedure. This will be done 1 to 2 weeks after the procedure.
What are some things patients do that make surgeons’ jobs harder? And what about those make it easier?
Some patients might come in with preconceived ideas which might come from doing research on online platforms that I have to correct. In addition to that, some patients might have heard from family or friends about treatments that may or may not apply to them.
Let me take the opportunity to tell you not to take supplements or traditional medicine that is not prescribed to you. If you take additional supplements or traditional medicine, it can interfere with the treatment.
Lastly, some patients doctor hop, which might confuse them and give them too many opinions. While this sounds good, it can lead to ‘analysis paralysis’, where we have too many choices to pick from.
I do think sometimes they may be looking for doctors which tell them what they want to hear, which may cloud the doctor’s opinion. All in all, I believe that doctors recommend treatments in the patient’s best interest.
Do you observe any colorectal-trends in Singapore?
In fact, we are starting to see more young people developing cancer in Singapore. To tackle this problem, the healthcare system in Singapore has set in place screenings which young people are encouraged to go for too.
The Ministry of Health in Singapore suggests starting to screen at the age of 50 if you have no strong risk factors.
For those with a family history of colorectal cancer, doctors will recommend screening at an even younger age. However, you should bear in mind that screening simply means that you are completely symptom-free and are just doing a health check.
If you have symptoms at any age, you should immediately inform your doctor so that you can get yourself checked. Detection of early stages of colorectal cancer can help to slow progression down and, in some cases, prevent it from getting more severe.
What challenges do colorectal surgeons face in Singapore?

The most challenging postoperative surgical complications I see after colorectal surgery are surgical site infection, anastomotic leakage, intraabdominal abscess, ileus, and bleeding. Each complication has a different influence on the outcome and has to be diagnosed accurately. Postoperative evaluation is necessary in order to achieve such quality requirements. [1]
Colorectal operations should be clean-contaminated procedures, which just means that these operations on sensitive and often messy areas are not contaminated. But there are times where there is contamination of both the peritoneal cavity and the surfaces of the surgical wound. Plus, large bowel diseases that require surgery tend to affect elderly patients.
A leak of luminal contents from a surgical join (Anastomotic leakage) after colorectal surgery may be divided into those which are clinically significant and those which are not.
Leakages occur in 3.4-6% of all colorectal cases. It is most commonly associated with rectal anastomosis, being clinically significant in 2.9-15.3% of cases. [2]
Usually, postoperative bleeding after colorectal procedures is a rare complication. The risk depends on the performed surgical procedure, the co-morbidities of the patient and in individual cases on an impaired clotting system.
In the initial postoperative phase, abnormal heart rate and low blood pressure should be reported and interpreted by the surgeon. Haemoglobin and hematocrit measurements can help to determine blood loss. [3]
A malfunction of intestinal motility after major intra-or extra-abdominal surgery (Postoperative ileus) has long been considered an inevitable consequence of gastrointestinal surgery. It prolongs hospital stay, increases morbidity, and adds to treatment costs.
The pathophysiology of postoperative ileus is multifactorial. The operating time and intraoperative blood loss are independent risk factors for postoperative ileus. [4]
Also read: How successful is colon cancer surgery, and what are the risks?
When should I visit a colorectal surgeon?
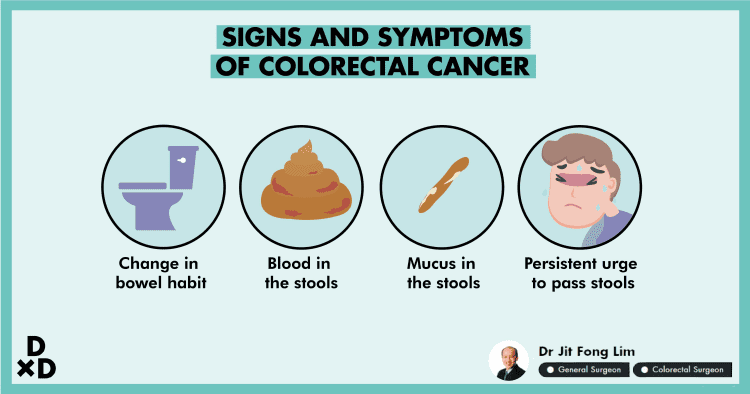
You should make an appointment with a colorectal surgeon if you have any of these symptoms or conditions:
- Changes in bowel habits
- Blood in the stools
- Mucus in the stools
- A constant urge to pass stools
What procedures do colorectal surgeons perform?
There are 7 treatments under colorectal surgery, called Laparoscopic surgery, robotic surgery, Transanal TME, Lateral pelvic lymph node dissection, preoperative therapy, adjuvant chemotherapy and radiotherapy. [5]
1. Laparoscopy surgery
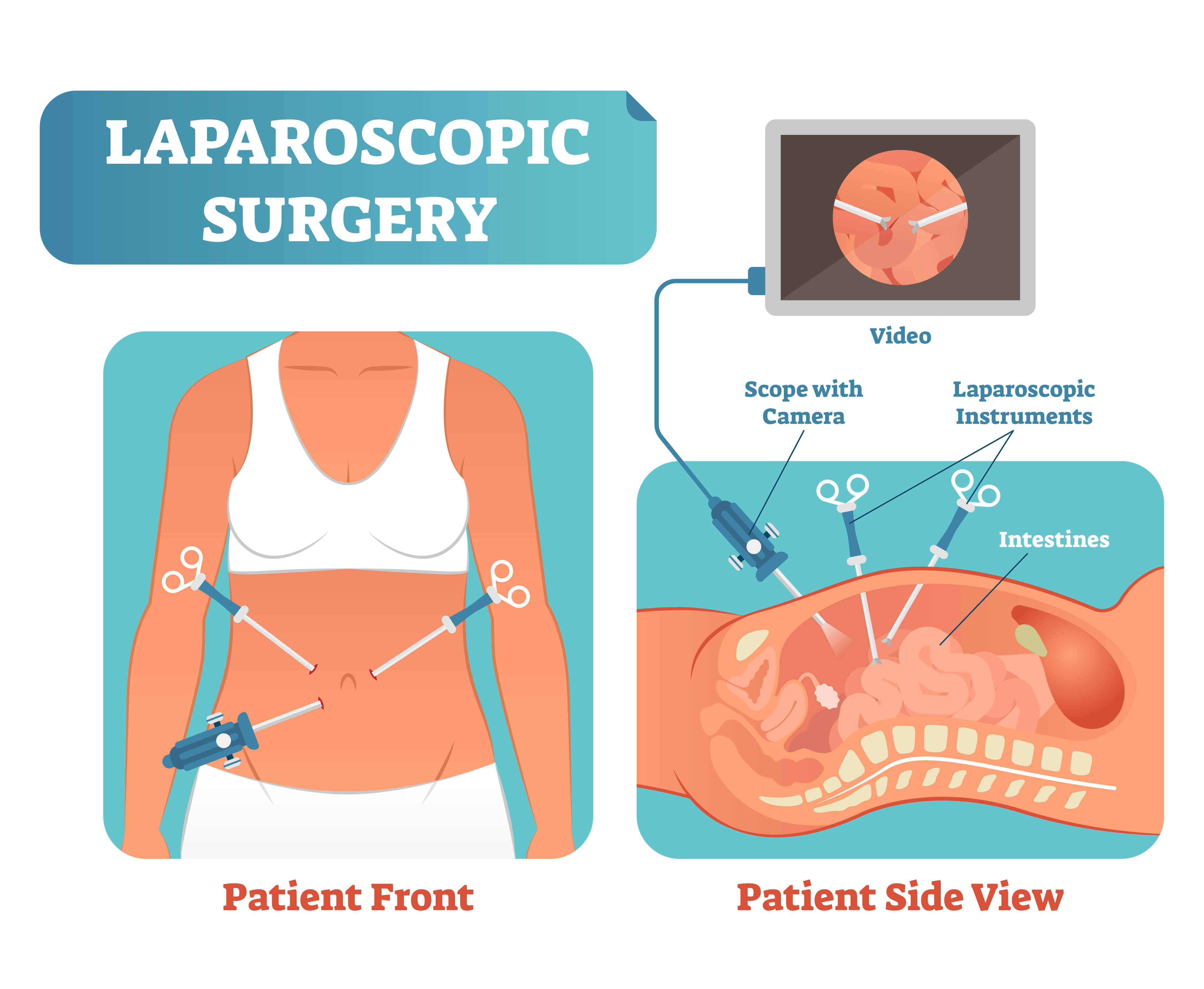
Laparoscopy, also known as keyhole surgery, allows the surgeon to carry out operations through four or five small (one-centimetre) cuts in the abdomen (tummy). A telescope camera, put into one of these small cuts, shows an enlarged image of the internal abdominal organs on a television screen.
The other cuts allow the surgeon to use special operating instruments. In some cases, one of the cuts may be made longer (to eight to 10 cms) to allow a bowel specimen (sample) to be removed and the procedure to be finished.
2. Robotic surgery
Robotic surgery is performed using various techniques, with or without laparoscopic surgery. Because the result of this surgery is reported to be similar to or less favourable than those of laparoscopic surgery, the learning curve for robotic colorectal surgery remains controversial.
Nonetheless, robotic colorectal surgery is practical and effective compared with traditional surgery, based on short and long-term oncological outcomes.. [6]
3. Transanal Total Mesorectal Excision (TaTME)
TaTME is a technique that combines an abdominal and transanal endoscopic approach to overcome limitations and facilitate standard laparoscopic TaTME. it is the ideal approach for patients with mid or low rectal cancer (within 8 cm from the anal verge).
Typically the treatment begins with the abdominal laparoscopic technique to examine the peritoneal cavity (presence of adhesions, carcinomatosis, pelvic anatomical characteristic, etc). [7]
4. Lateral pelvic lymph node dissection (LPLND)
LPLND may be therapeutic in the presence of enlarged lateral pelvic nodes or may present disease (be prophylactic) in the absence of any obviously enlarged lateral pelvic nodes.
It is hypothesized that LPLND removes those nodes that contain small collections of cancer cells (micrometastasis). This then decreases the development of recurrence in that area.
5. Preoperative therapy
Preoperative therapy in the management of rectal cancer has been gaining ground in Europe and the US. Many potential advantages make preoperative therapy an attractive strategy. [8]
6. Chemotherapy

Chemotherapy or chemo is often used to treat colorectal cancer. It is the use of drugs to kill cancer cells. Chemo drugs attack fast-dividing cells quickly, which is why they work against cancer cells.
But other cells in the body, such as those in the bone marrow (where new blood cells are made), the lining of the mouth and intestines, and the hair follicles, also divide quickly. These cells can be affected by chemo too, which can lead to side effects.
7. Radiotherapy
In order to kill cancer cells, radiotherapy requires high-radiation (such as x-rays) or particles. It is more often used to treat people with rectal cancer than for people with colon cancer. Treating with chemotherapy at the same time will help radiation therapy perform better on some colon and rectal cancers.
Read also: What is the possibility that cancer will recur even after a colorectal surgery?
What tests fall under colorectal surgery?
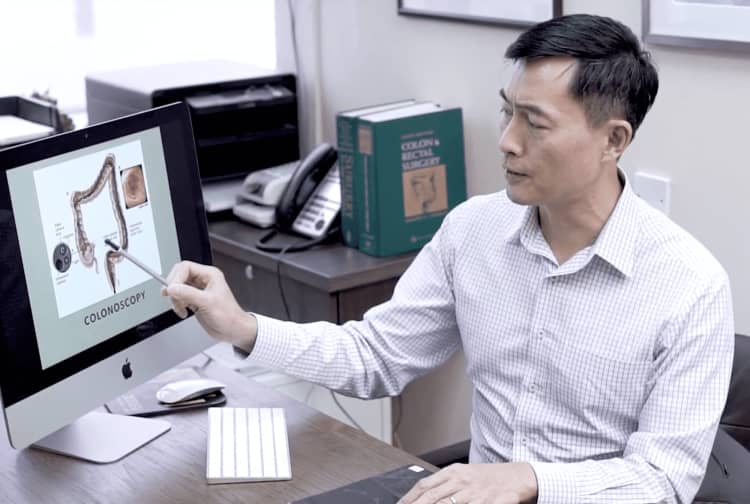
1. Colonoscopy
Colonoscopy is one of several screening tests for colorectal cancer. I use a long, thin, flexible, lighted tube to check for polyps or cancer inside the rectum and the entire colon. During the test, I can find and remove most polyps and some cancers.
Colonoscopy is also used as a follow-up test when something suspicious is found during one of the other tests.[9]
2. CT colonography
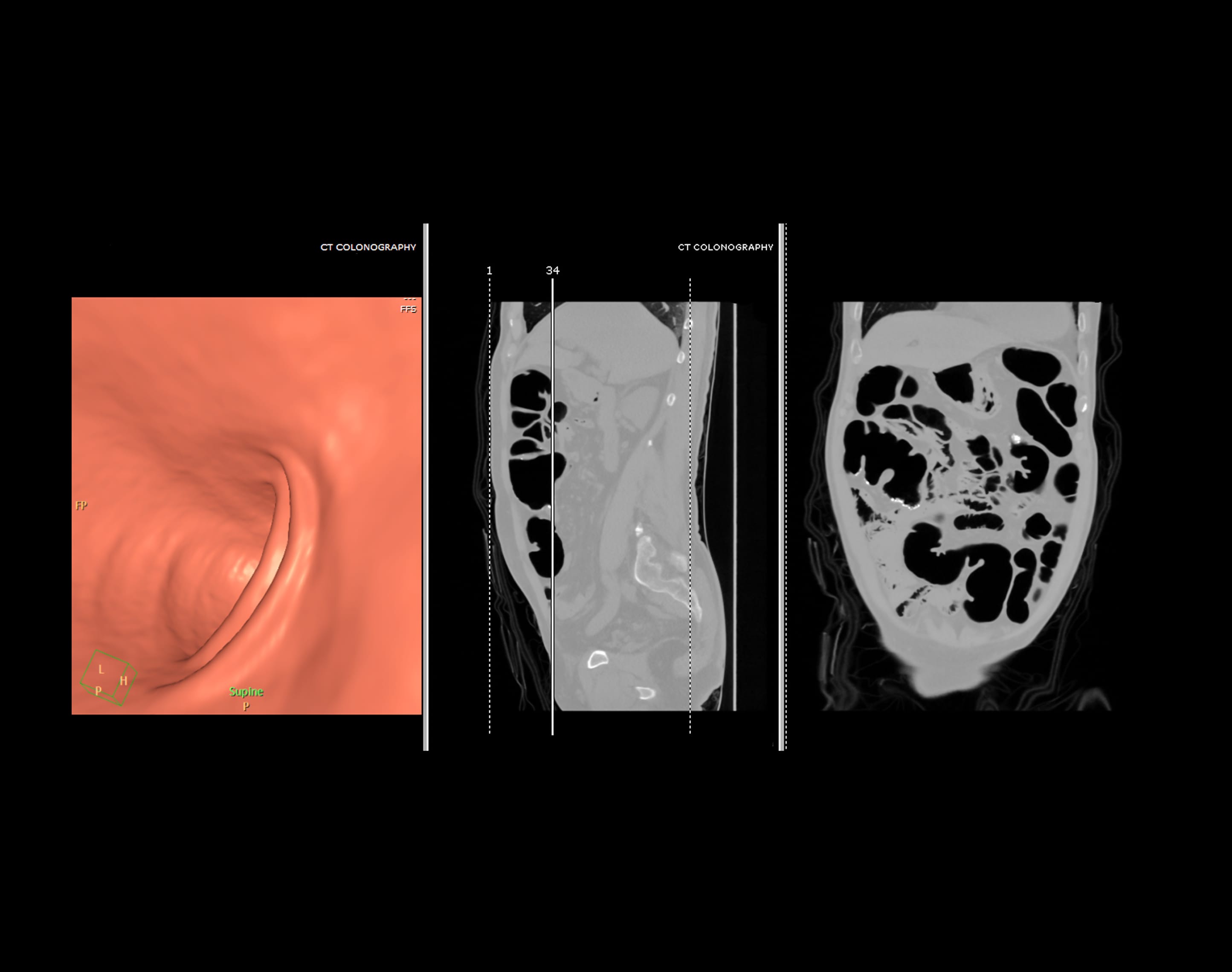
Computer tomography (CT) colonography, sometimes known as simulated colonoscopy, utilizes x-rays and machines to generate photographs of the whole colon, which is projected on a doctor’s computer screen for examination.
3. Faecal immunochemical tests
The faecal immunochemical test (FIT) is a screening test for colon cancer. It tests for hidden blood in the stool, which can be an early sign of cancer.
FIT only detects human blood from the lower intestines. Medicines and food do not interfere with the test. It thus appears to be more reliable and has less false-positive outcomes than other studies. [10]
4. Barium enema
A barium enema is an x-ray of the colon and rectum. The rectum and colon make up the large intestine that lets your body control waste. A barium enema helps doctors find health conditions in the colon and rectum, such as
- Inflammation
- Polyps,
- Cancer.
Barium is a contrast medium. A contrast medium is a substance used to make clearer images of the inside of the body.
5. Flexible sigmoidoscopy
This test is an effective screening technique because it is capable of identifying early improvements in the distal colon. The 60-cm adjustable sigmoidoscope provides patients with superb visualisation and reduced pain.
Successful sigmoidoscopy requires appropriate care of the patient, proper equipment and a skilled doctor who can distinguish both usual and irregular outcomes.
Complications arising from sigmoidoscopy are rare but patients may experience some cramping, gas, or watery stools. Screening and primary preventive measures, including regular exercise and increased dietary fibre intake, can lower the morbidity and mortality associated with colorectal cancer.
How much does colorectal cancer surgery cost in Singapore?
The price can vary because there is an additional charge for:
- The procedure itself
- The instruments used for the procedure
- The pathology laboratory cost.
Since the expense depends on the complexity of the situation and the procedure used, prices range from $40,000 to $70,000 on average.
Colorectal cancer is complicated and a team of doctors, nurses, and advanced equipment is needed. You need to stay in the hospital for around 7 to 10 days after the treatment.
How do I find the best colorectal surgeon for me?

In my opinion, word of mouth recommendations are the most effective. Do also go through online reviews and do your own research. However, there is also nothing wrong with going straight to proctologists to get the treatment done.
There are a few specialized and general hospitals in Singapore where the best colorectal surgeons in the region diagnose the disease and perform this type of surgery. Why don’t you book an appointment at Human?
Are colorectal cancer surgeries Insurance or Medisave-claimable?
Colorectal cancer surgery is Medisave and insurance claimable. It would be best to contact your insurance provider as they are the best persons to answer your policy questions.
Are there any questions you encountered that you would like to share?
Does a colonoscopy hurt?
I tell my patients that a colonoscopy can be made completely painless provided that the doctor has experience while also providing due care. When you have it done with an experienced doctor, the procedure can be smooth and relatively pleasant.
Is colorectal cancer curable?
In most cases, colorectal cancer is curable. If you have an early stage of colorectal cancer, the chance of recurrence is very low after treatment. Those with advanced stages of cancer are generally harder to treat. Therefore, early screening and detection are important.
Healthy Diet and Active lifestyle is the way to go!
A good diet and lifestyle can help reduce your risk of developing colorectal cancer. However, even with a good diet and a healthy lifestyle, you should go for colorectal cancer screenings when you reach 50 years old.
If you feel some of the symptoms above, such as having blood in your stools, changes in your bowel habits, mucus in the stool, or maybe persistent urge to pass stools, why don’t you book an appointment with your doctor to get the right test and treatment?