Glaucoma is one of the leading causes of blindness in the world. It accounts for 6 million of the estimated 40 million blind in the world and is the leading cause of irreversible blindness worldwide. In Singapore, Glaucoma accounts for 40% of blindness in Singapore.
“UP TO 50% OF ALL PEOPLE WITH GLAUCOMA IN SINGAPORE ARE NOT AWARE THEY HAVE THE CONDITION. HOWEVER, IF IT IS DIAGNOSED EARLY, TREATMENT CAN BEGIN AND VISION LOSS CAN BE PREVENTED”. – Dr David Goh
Glaucoma affects 3% of people over the age of 40 and 7% over 70 years of age. However, early-onset Glaucoma can also occur to people under the age of 40 and it is usually hereditary. The abnormalities that block your trabecular meshwork can be present from birth.
Patients often come to me and say “I can't have Glaucoma because I can still see clearly. I do not feel pain and everything seems normal to me”. This is because Glaucoma does not always have symptoms, especially during the early stages.
As an ophthalmologist for more than 20 years, I have written this article to share some of my knowledge about Glaucoma. In this article, I will cover in a Q&A style, the following:
- Definitions
- Symptoms
- Risk factors
- How to diagnose Glaucoma
- Glaucoma treatments available
- Glaucoma surgery, including minimally invasive (MIGS) and Conventional drainage surgery
Read More: The Ultimate Guide to Age-related Macular Degeneration (AMD) in Singapore (2020).
What is Glaucoma?
Glaucoma is commonly known as the ”silent thief of sight” because it can cause irreversible vision loss without any obvious symptoms.
The term Glaucoma refers to a disease that lead to eye (optic) nerve damage, the nerve fibres that transmits signals from the eye to the brain to produce the image that we see.
When a significant part of the nerve is damaged, your peripheral ( side) field of vision is lost - this vision loss gradually extends towards your central vision, until eventually all sight is lost. Vision loss caused by glaucoma is permanent.

What are the Types of Glaucoma in Singapore?
There are 2 major types of Glaucoma:
1. Open-angle Glaucoma
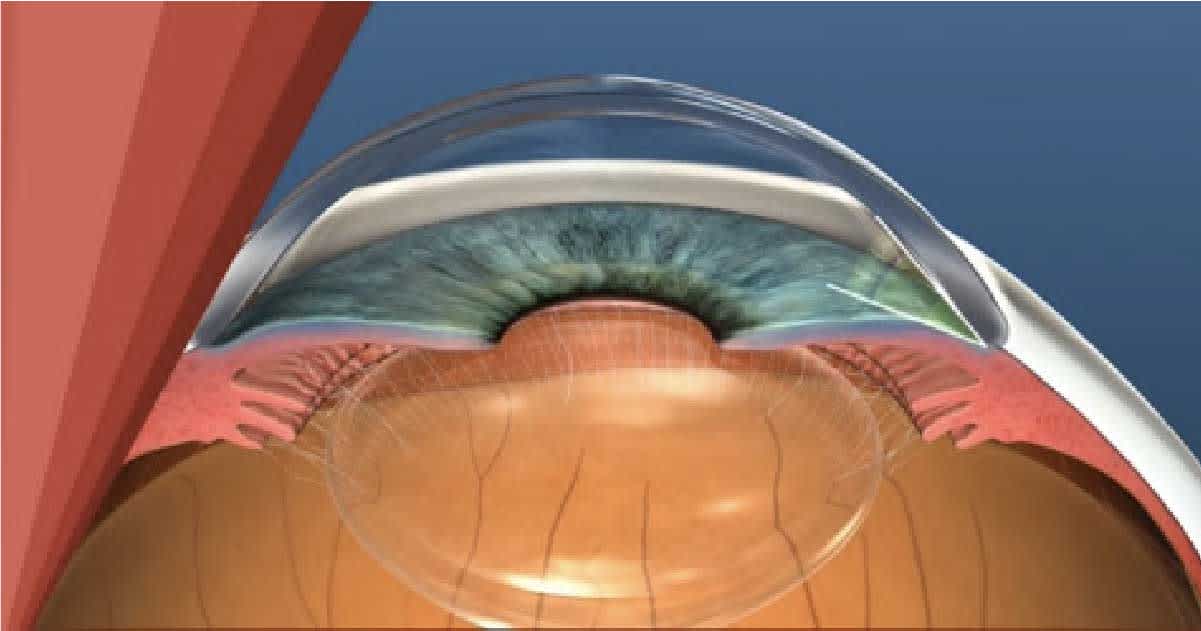
The most common form of the disease. The drainage angle formed by the cornea and iris remains open but the trabecular meshwork is partially blocked, resulting in the builds up of the eye pressure and damage the optic nerve.
This type of glaucoma is painless and causes no vision changes at first. Regular eye check-ups are essential to find early signs of damage to the optic nerve.
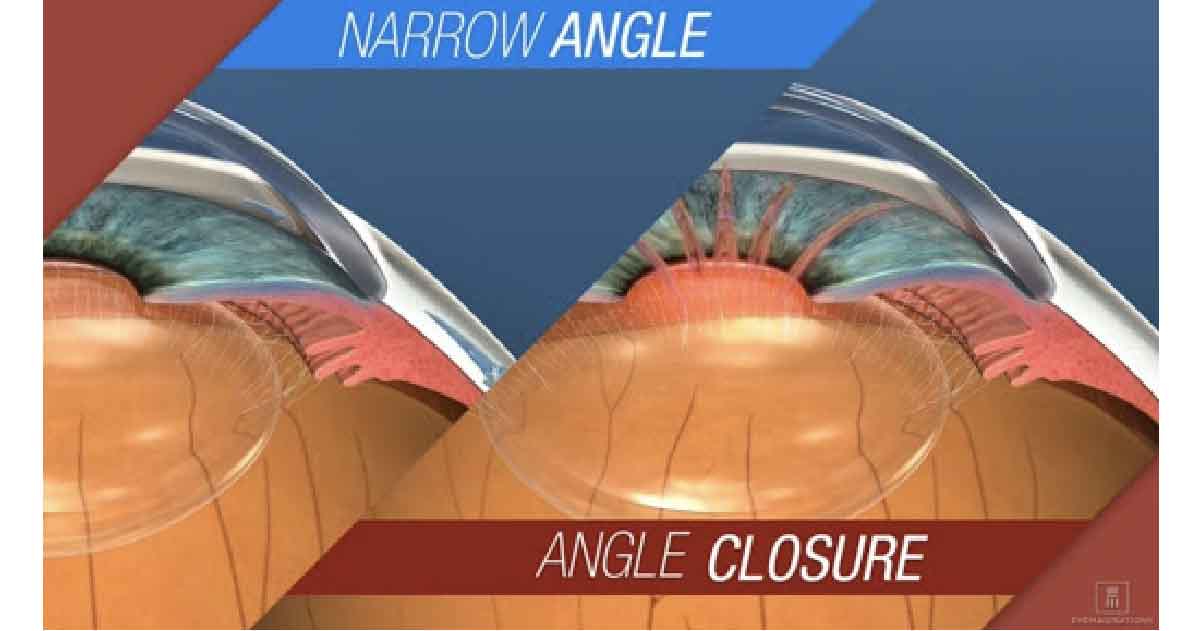
2. Angle-closure Glaucoma / Closed-angle Glaucoma / Narrow-angle Glaucoma
This occurs when the iris bulges forward to narrow or block the drainage angle formed by the cornea and iris, thereby causing the fluid cannot circulate through the eye and IOP increases. It may occur suddenly as acute attack or gradually as chronic angle-closure glaucoma.
An acute attack happens when the drainage angle gets completely blocked and the IOP rises drastically. It is a medical emergency and can be triggered by sudden dilation of your pupils.
Chronic angle-closure glaucoma doesn't present symptoms at first, so the patient might not realize until the damage is severe or get attacked. Angle-closure glaucoma can cause blindness if not treated right away.
What are the symptoms of Glaucoma?
Different types of Glaucoma have different symptoms. While the symptoms of open-angle Glaucoma are not apparent at first, the symptoms of closed-angle Glaucoma are considered a medical emergency and have to be treated quickly.
Some of the symptoms that occur are: [1]
Open-angle Glaucoma
- A gradual loss of side vision
- The advanced stages include tunnel vision, meaning you can only see things when they are right in front of you
Closed-angle Glaucoma
- Severe eye pain that causes nausea and vomiting
- Blurred vision
- Eye redness
- Seeing halos around objects
- Sudden vision disturbance, usually in dim lights
What are the risk factors for developing Glaucoma?
- Advanced age (>40)
- Genetics (having family member with glaucoma)
- African, Asian ( Chinese) or Hispanic heritage
- Have high eye pressure.
- Severe myopia (short-sightedness) or hyperopia (long-sightedness).
- Have had an eye injury.
- Have corneas that are thin in the centre.
- Have thinning of the optic nerve.
- Have diabetes, migraines, poor blood circulation or other health problems affecting the whole body
- Heart disease
- High blood pressure
- Sickle cell disease
How Glaucoma diagnosed in Singapore?
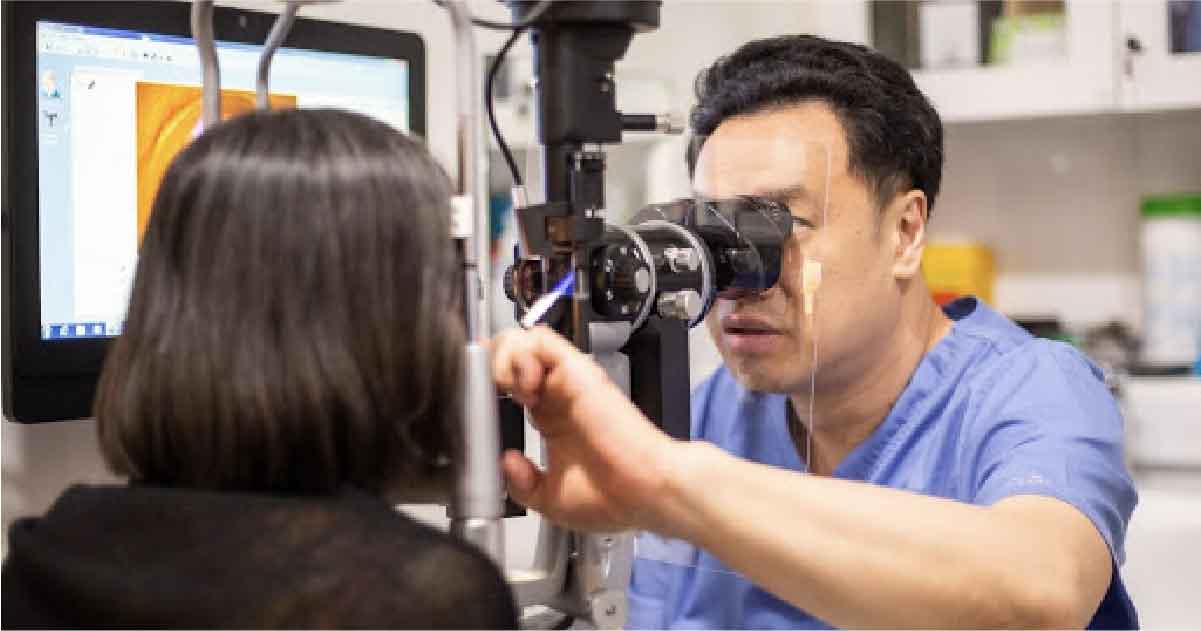
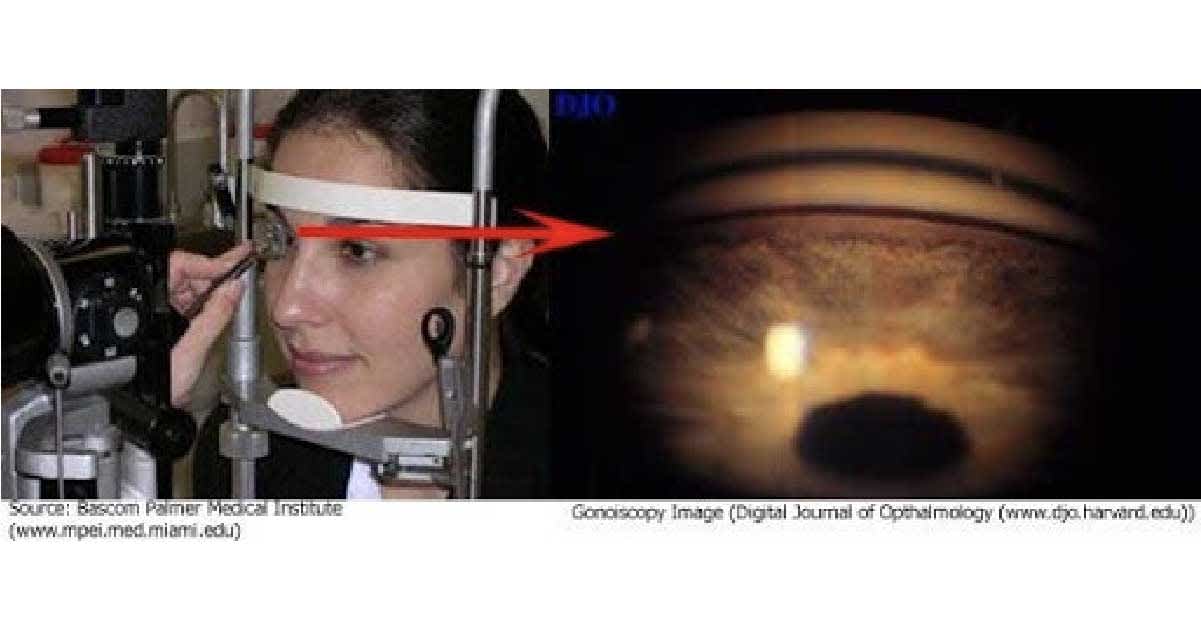
In order to know how to diagnose Glaucoma, you need to see your ophthalmologist and take a specific examination like tonometry and visual field testing. During this examination, your ophthalmologist will: [2]
- Take a measurement of your eye pressure
- Inspect your trabecular meshwork’s angle
- Examine your optic nerve to see if there is any damage
- Test your side vision
- Take a visual examination of your optic nerve
- Measure the thickness of your cornea
You should start getting a baseline eye screening for Glaucoma at the age of 40 onwards because early signs might occur at this age. Usually, your doctor will tell you how often you should get your eyes checked after you get your baseline result. However, if you have chronic:
- Diabetes
- High blood pressure
- Steroid usage
You need to have your eyes checked earlier because you are at higher risk of developing early-onset Glaucoma. [3]
Usually, Chinese people have a higher risk of developing Glaucoma compared to Malay people and Indian people, especially women.
Why do certain ethnicities have higher or lower chances of getting Glaucoma?
There is no actual reason why certain ethnicities have a higher risk of developing Glaucoma. Unfortunately, Chinese ethnicities are more prone to have bad eyesight. If you are a Chinese woman, you will have a higher risk of developing Glaucoma compared to other ethnicities.
The East Asian population are generally more prone to developing closed-angle Glaucoma due to the anatomy of their eyes. Generally, the eyes of east Asian people are more narrow with less of their trabecular meshwork exposed. Therefore, there is a higher risk of having it blocked. [4]
In addition, Singapore has one of the highest rates of myopia, especially in children, and one of the highest rates in the world for Glaucoma as well.
How is Glaucoma Treatment conducted in Singapore?
Glaucoma treatment often starts with prescription eyedrops. It works either by reducing the production of the aqueous fluid or by increasing the drainage of the fluid out of the eye. There is a multitude of different eyedrops which once started, usually have to be continued life-long.

However, eye drops have side effects if they are used too much. For instance, you can experience redness or allergic reactions. Once you start using eye drops for Glaucoma, you can also become dependent on it and can become more expensive in the long run.
Also read: Why is it important to use prescription eye drops for Glaucoma at the same time each day?
Laser Treatment for Glaucoma
Besides, there are three main types of laser therapy for glaucoma to help aqueous drain from the eye and usually done in the ophthalmologist’s office or an outpatient surgery centre.
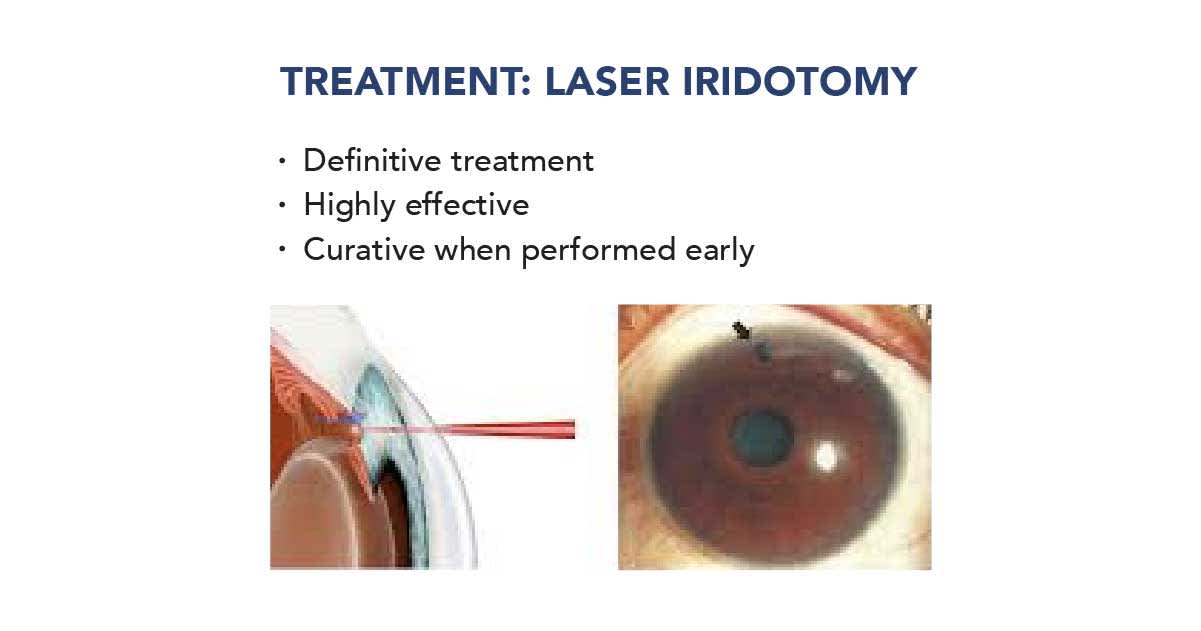
Laser iridotomy is applied for people who have angle-closure glaucoma. It involves making a hole in the iris by laser to allow fluid to drain normally in eyes and reduce the eye pressure.
Meanwhile, laser trabeculoplasty is used to treat people who have open-angle glaucoma. This procedure is a quick, relatively painless, and safe method of lowering the IOP. In some cases, it is used as the initial or primary therapy for open-angled glaucoma.
With the eye numbed by anaesthetic drops, the laser treatment is applied through a mirrored contact lens to the angle of the eye. Microscopic laser burns to the drainage angle, allowing fluid to be drained away more effectively. However, the effect of laser trabeculoplasty can only last about two years.
There are 2 types of laser trabeculoplasty: argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT).
Many reports suggest that both ALT and SLT have similar IOP-lowering effects, however there are many problems associated with ALT, including irreversible damage to the eye, along with permanent scarring in the angle. In contrast, SLT is less likely to produce scarring in the angle, thus it can be repeated multiple times.

Laser Trabeculoplasty (SLT)
Laser cyclo-ablation (also known as ciliary body destruction or cyclophotocoagulation) is another form of laser therapy applied for patients with severe forms of glaucoma with poor visual potential.
This procedure involves applying laser burns to the ciliary body, the part of the eye that produces the aqueous fluid, destroying the cells that make the fluid, thus reducing the eye pressure. It is performed after other traditional therapies have failed.
Besides laser therapy, there are some glaucoma surgeries which are done in an operating room. Trabeculectomy is a filtering surgery where a tiny flap is created in the sclera (white of the eye) and part of the trabecular meshwork is removed.
A bubble (like a pocket) will also be created in the conjunctiva which is known as a filtration bleb. It is usually hidden under the upper eyelid and cannot be seen. Aqueous humor could be drained out of the eye through the flap and into the bleb. In the bleb, the fluid is absorbed by tissue around your eye, thus lowering eye pressure.


On the other hand, the eye surgeon could insert a tiny drainage tube shunt in your eye to create a new pathway for fluid to exit the eye. The fluid is then sent to a collection area (reservoir) beneath the conjunctiva and absorbed into blood vessels nearby.
In recent years, minimally-invasive glaucoma surgery (MIGS) involves various devices such as the i-Stent inject, the Hydrus Microstent, the InnFocus Microshunt, have shown promising results.
MIGS mainly refers to the procedures that are bleb-independent, including trabecular bypass stents and supra choroidal shunts, which aim to prevent the major bleb-related complications.
It is directed at creating openings in the trabecular meshwork, the drainage ring in the wall of the angle of the eye, providing an alternate surgical procedure in lowering eye pressure.
To date, the iStent and Trabectome are FDA-approved and have shown modest short term IOP lowering especially when combined with cataract surgery. Nowadays, these MIGS are less invasive, one of them being the iStent-inject.
iStent is a minimally invasive glaucoma surgery (MIGS) using a tiny titanium device and works to increase the outflow drainage from the eye.
If you have mild or moderate Glaucoma, our preferred treatment would be minimally invasive Glaucoma surgery such as iStent-inject. Watch the video here.
What method of treatment is preferred by doctors for Glaucoma in Singapore?
The least invasive and standard treatment for Glaucoma is using eye drops. However, eye drops have side effects if they are used too much. For instance, you can experience redness or allergic reactions. Once you start using eye drops for Glaucoma, you can also become dependent on it. Therefore it can become more expensive in the long run.
Other extreme major bypass surgeries are either called tubectomy or tube drainage surgery to drain the fluid away and are reserved for advanced and serious cases of Glaucoma.
If you have mild or moderate Glaucoma, our preferred treatment would be minimally invasive Glaucoma surgery such as iStent. This is because even though the procedure costs a lot at first, you do not have to spend more money on eye drops, which means it is more economical in the long-term.
Are there any lifestyle habits I can change to prevent Glaucoma?
Glaucoma generally affects 3% of people over the age of 50 and 7% of people over the age of 70. However, even though not proven, these habits may help prevent Glaucoma: [5]
- Get your eyes checked regularly. It can help detect Glaucoma early, therefore you can find the best way of slowing down the symptoms before it gets worse
- Wear shades to prevent your eyes from the UV rays
- Exercise but not too much as it can increase the production of eye fluids that lead to the failure of your trabecular meshwork to drain the fluids
- Moderate your caffeine intake. Too much caffeine can increase the production of your eye fluids that might damage your trabecular meshwork
I have Glaucoma. What can I do to improve my quality of life?
Unfortunately, Glaucoma damage cannot be reversed. Surgeries or treatments can only prevent the condition from getting worse. The only way to improve your quality of life is by improving your visual aid, such as:
- Wear prescribed spectacles so you can see better
- Make your light bright at home
- Be more aware of your surroundings to minimise tripping over things
If you have both cataracts and Glaucoma, I would advise you to remove the cataract as it can improve your overall quality of vision. Therefore, your quality of life will also be better.
Are the Glaucoma treatments Medisave-claimable?
Unfortunately, Glaucoma medications are not Medisave-claimable. Therefore, you have to pay for the medications at full price.

Conclusions
Vision loss in Glaucoma is inevitable if left untreated but you can still slow or stop the progression of Glaucoma if it is diagnosed early. Even though it mainly occurs to people over the age of 50, younger people can also develop Glaucoma.
Make sure that you are handled by professionals to minimise the chance of complications that might occur if you opt for the minimally invasive treatment.
Do ask your trusted eye doctors if you have any more questions regarding Glaucoma.
Hope this article helps! Read more about glaucoma and get a quote for treatment/consultation with a doctor.
Dr David Goh is a medical director of Novena Bladeless Cataract surgery & Eye specialist centre. He specialises in Bladeless Laser Cataract surgery, simple and complex Glaucoma and general ophthalmology. He spent 20 years in the UK where he completed his Medical studies and basic Eye surgical training in Ophthalmology.
He then completed his Higher Ophthalmology surgical training and Specialist Fellowship at the world renowned Moorfields Eye Hospital, London, before returning to Singapore. He has previously worked in Singapore National Eye Centre ( 2010 – 2017 ) as a consultant in Glaucoma, Cataract and Comprehensive Department.