Did you know that between 2010 and 2013, 386,226 women had done a hysterectomy in the United States? [1] In fact, hysterectomy remains to be one of the most common surgeries that Singaporean women go through.
As a gynaecologist myself, I would love to help clear up some of the doubts surrounding hysterectomy. At the same time, I would like to help you find the best form of treatment that works best for your case.
Here are a few key points that you should know about hysterectomy. Read on to find out!
Read more about menopause and how to treat its symptoms here!
What is a Hysterectomy?
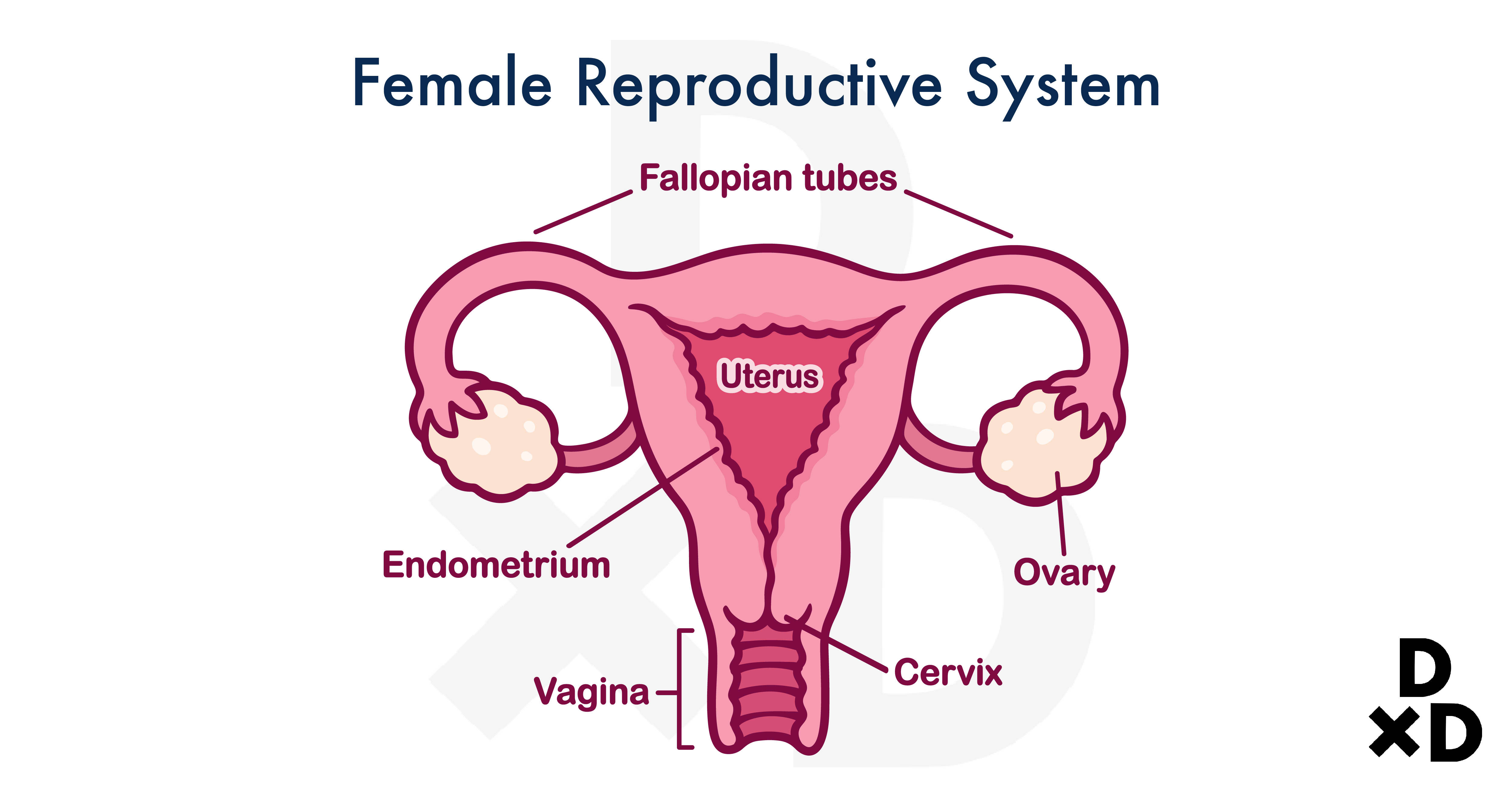
A hysterectomy is a surgery done to remove the uterus from a woman.
A quick refresher for those of you who forgot what you have learned from science class! The uterus, also known as the womb, is where a foetus grows in a pregnant woman.
Usually, you will have your whole uterus removed. However, it depends on the type of hysterectomy you receive. It is common to have your fallopian tubes and ovaries removed as well [2].
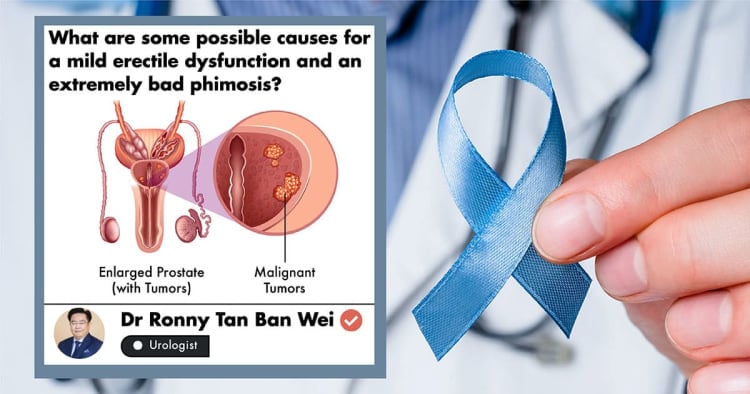
Why do women need Hysterectomy?
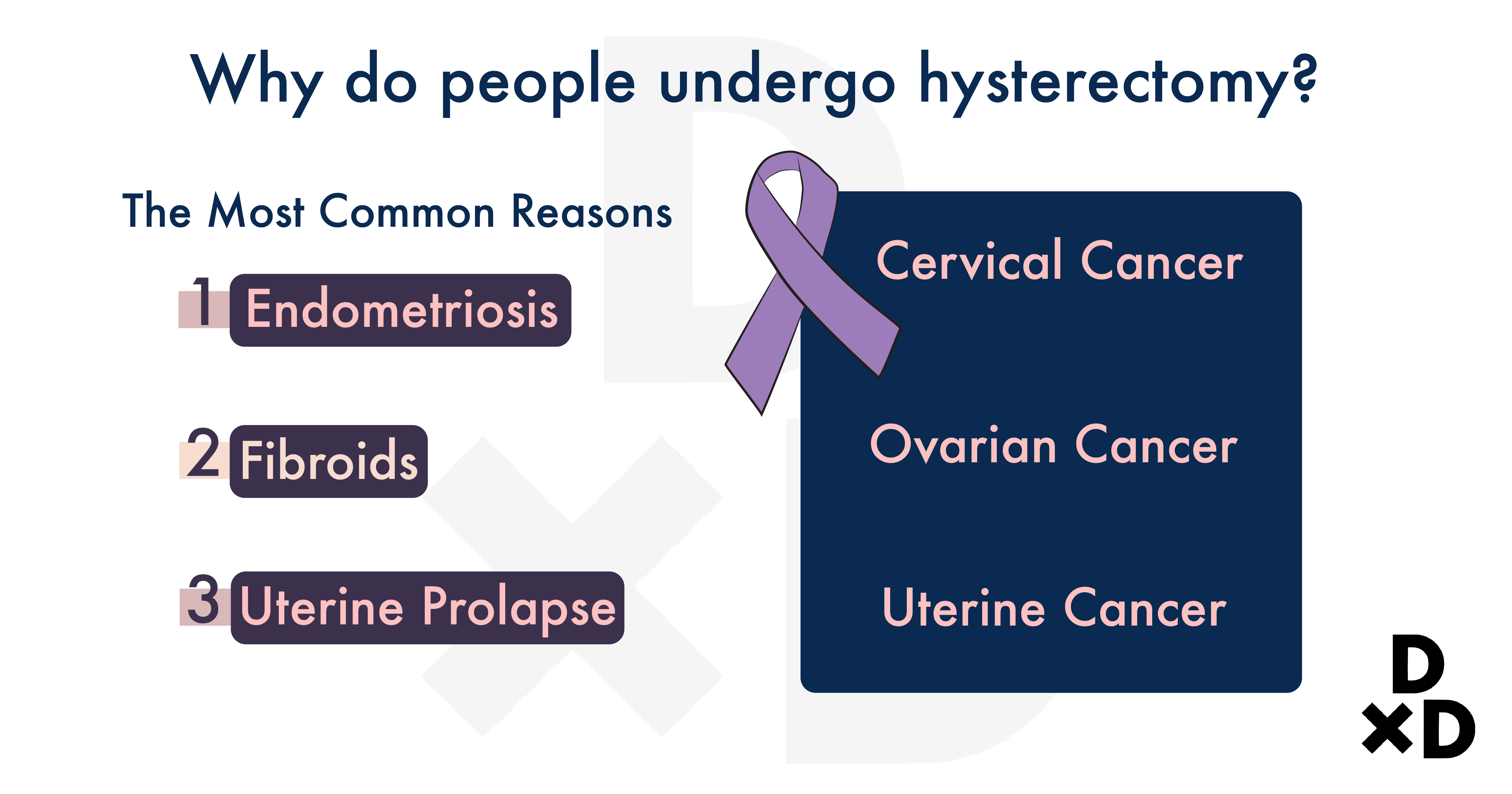
There are a few reasons for women to get a hysterectomy done: [2]
- One, they help to treat non-cancerous conditions which affect most women.
- Two, they also help treat cancerous conditions.
The first one forms a large part of the reason why many women have done a hysterectomy. Out of these, the more common reasons are found to be caused by:
On top of that, you should also get a hysterectomy done if you have:
- Heavy and irregular menstrual bleeding
- Severe menstrual pain
- Cancer of the cervix, uterus, and ovary
Let's find out in detail what these conditions are.
Related: The Ultimate Guide to Cervical Cancer in Singapore (2021)
1. Endometriosis or Adenomyosis
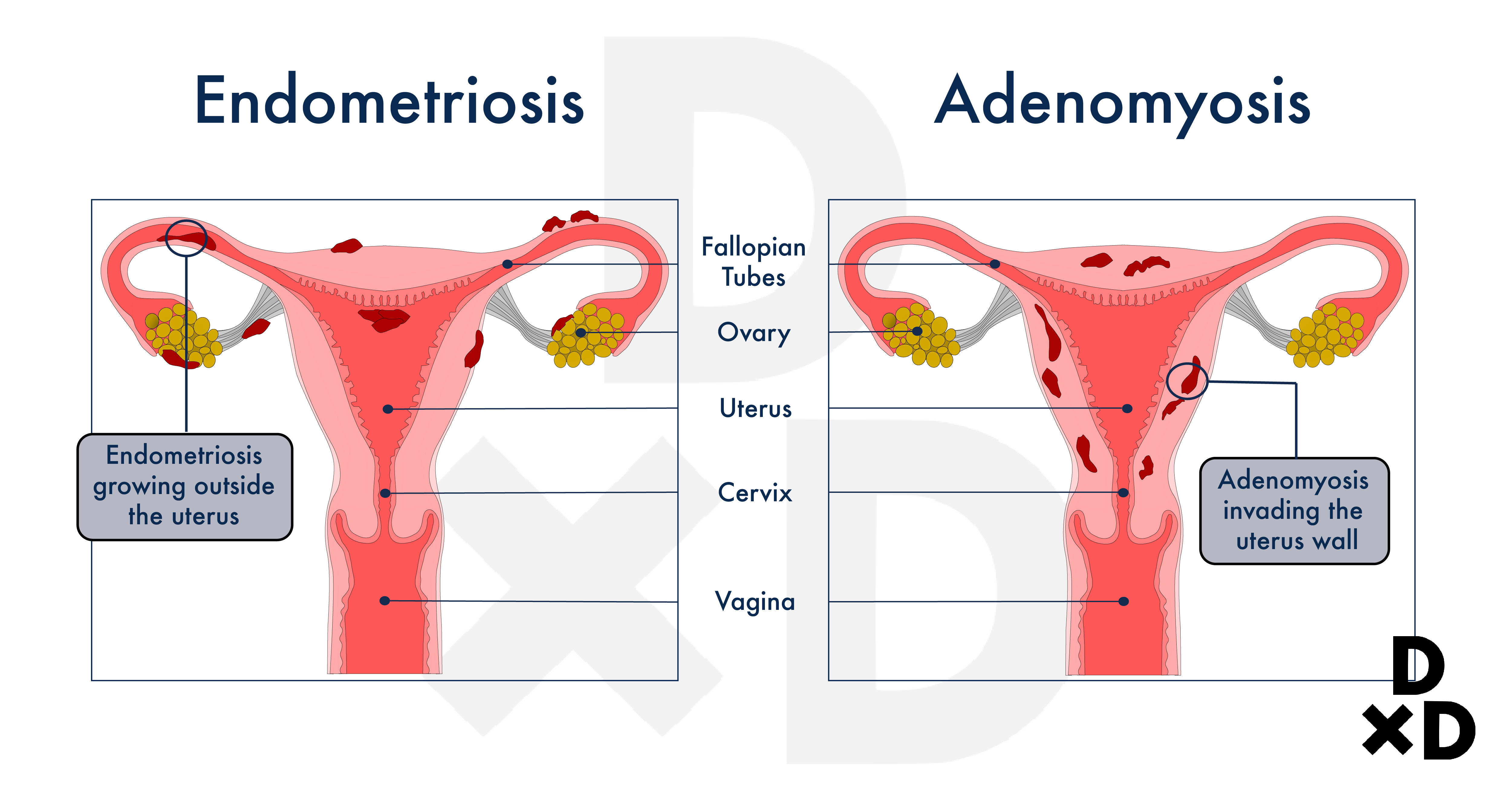
Endometriosis happens when the cells from the lining of the womb grow outside the womb. This layer of lining is also known as the endometrium [3].
Very often, the growth of the endometriosis can be found in these areas, which are located outside the womb:
- Ovaries
- Fallopian Tubes
- The surface of the uterus
- The area behind the uterus, also known as, the Pouch of Douglas
- Bowel
- Bladder
- The ureters
- Rectum
You can read more about endometriosis here in our guide.
On the other hand, adenomyosis is slightly different. In adenomyosis, the cells from the lining of the womb break through the muscle layers of the uterus. As such, growth can be found at these muscle layers, which is also known as the myometrium [4].
While they are not cancerous conditions, it will be wrong to think that it is ok to leave them untreated. Leaving them untreated can put you in pain and discomfort. Read on to find out about their symptoms and how you can treat them.
How can I differentiate the two?
There are some common signs that can help you detect if you have any of the above conditions. If you suffer from endometriosis, you should look out for the following signs: [3]
- Painful menstrual periods
- Pain experienced during sexual intercourse
- Pain during urination or with any bowel movements
- Pelvic pain
- Infertility
- Fatigue, nausea, and diarrhoea especially during your period
On the other hand, if you have adenomyosis, you will spot the first two symptoms and three other symptoms which include: [4]
- Pelvic pain which lasts for a long time
- Irregular and prolonged menstrual periods
- An enlarged uterus
However, you should take note that not everyone experiences the same symptoms. Some women may not experience any, but some may have more severe symptoms.
Depending on the symptoms that you have, you may require different tests as well. For instance, if you show signs of pelvic pain, you may be required by your doctor to undergo tests to rule out other possible causes of pelvic pain. While the list is not exhaustive, some of the tests include:
- Physical examination and radiology tests
- Urine Tests
- Pregnancy Tests
Also read: What are the recent advances in treating adenomyosis?
How can I treat Endometriosis or Adenomyosis?
Medical treatments tend to be the first line of treatment. These treatments usually come in the form of pain relief drugs that can help ease the inflammation and pain they cause.
As both conditions are highly associated with pelvic pain and menstrual abnormality, certain hormonal medication may also help relieve the symptoms. Some examples include: [3]
- Hormonal contraceptives
- Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists
- Progestin therapy
They work by halting the production of hormones that causes menstruation. Through that, they decrease the menstrual flow or stop them as a whole.
I will recommend that you go for a hysterectomy only if other forms of treatments have not worked for you.
2. Fibroids
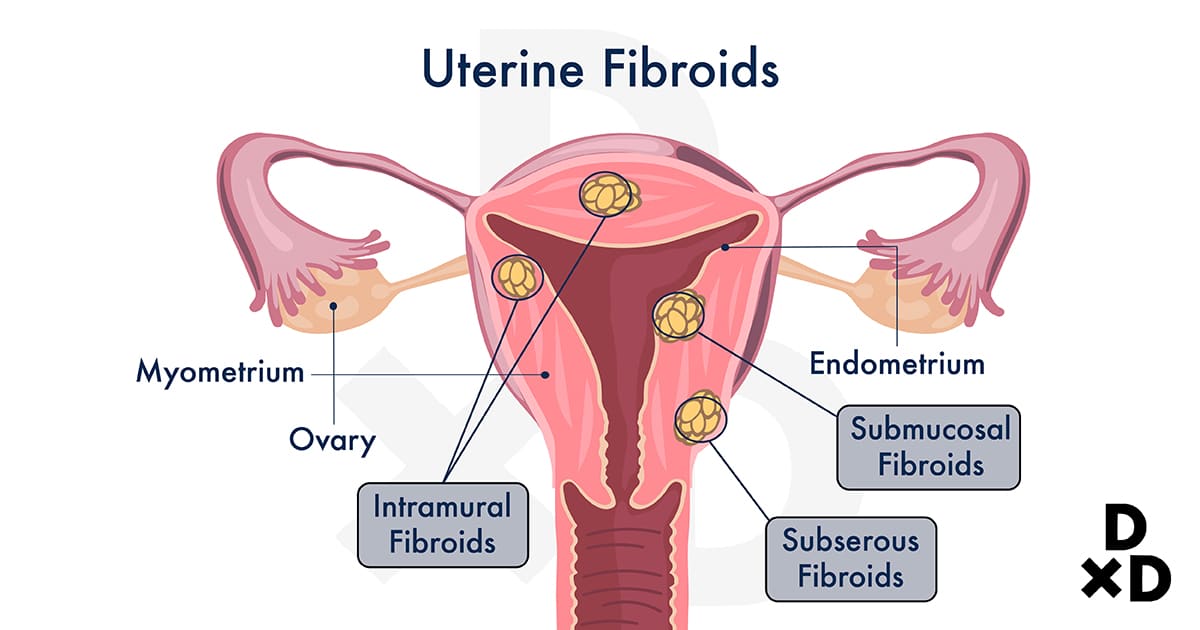
Fibroids can be found at the muscle walls of the uterus also known as the myometrium. In fact, many women have this condition. On top of that, the condition seems to be more common in women of childbearing age [5].
As a result, you are less likely to be diagnosed with fibroids if you fall under one of these age groups:
- Girls before puberty
- Women who have had menopause
In most cases, fibroids do not cause any problems as they are generally non-cancerous. There is a less than 1 in 1000 chance that a cancerous fibroid (called leiomyosarcoma) occurs [6]. However, that does not mean that you should leave them untreated!
What are some common signs of fibroids?
If you have fibroids, you are likely to develop the following symptoms: [6]
- Heavy or prolonged menstrual periods (more than 7 days)
- Pain or pressure on your pelvis
- Frequent need to go to the toilet
- Complications during pregnancy and labour
- Pain during sex
- Constipation
- Backache
To help you with your symptoms, you can first opt for non-surgical treatments. If those treatments did not help you much with the symptoms, your surgical options are to have the fibroids removed but preserve the uterus (myomectomy) or hysterectomy.
Also, you should seek your doctor's help for a hysterectomy procedure if you have fibroids that are:
- Too big to treat non-surgically
- [Rapidly growing](https://keystone.human.com.sg/keystone/What are my treatment options for fast growing fibroids) in numbers
- Potentially cancerous
Also read: Am I suitable for laparoscopic myomectomy fibroid removal if I have a large fibroid?
3. Uterine Prolapse
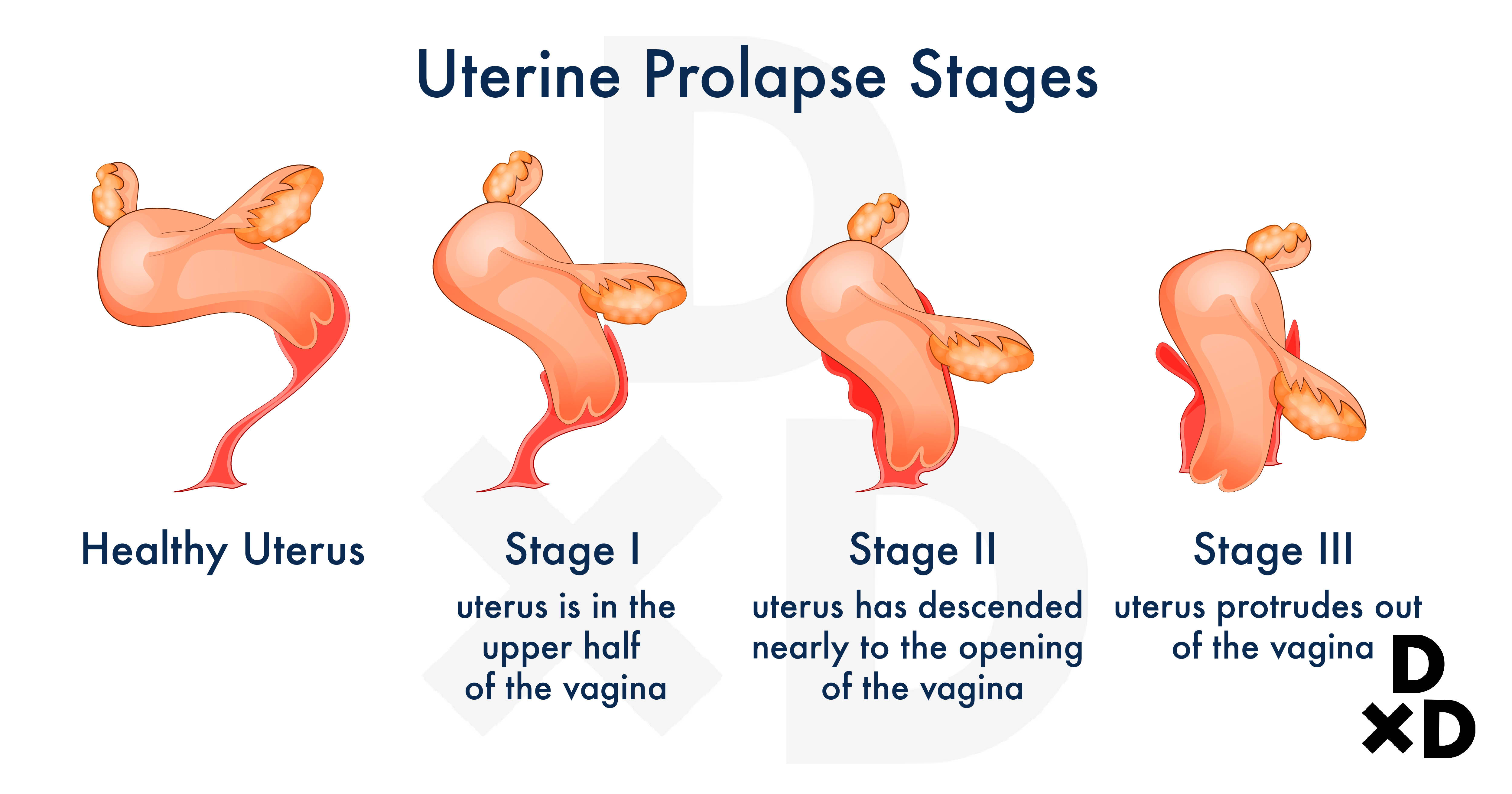
Uterine prolapse happens when the uterus droop into the vagina or in some cases, may even protrude out of it. Why does this happen? Let's find out!
The uterus is held up by a woman's pelvic floor muscles and ligaments. If you have uterine prolapse, it is probably a sign that your pelvic floor muscles have weakened [7].
While uterine prolapse can affect women of any age, it is more commonly found in women who fit the following descriptions:
- Gone through menopause
- Underwent several vaginal births (natural birth)
- Had difficulties with vaginal births
What are the causes and symptoms of uterine prolapse?
Besides the effects of gravity, you may get uterine prolapse from childbirth. This is because childbirth puts quite a strain and damage on your pelvic floor muscles and ligaments. In the case of post-menopausal women, it is most likely due to the lack of oestrogen [7].
If you have a mild degree of prolapse, you may not experience any symptoms at all.
However, if you have moderate to severe prolapse, you may feel like something is "falling" out of your vagina. Along with that, you may also experience these other symptoms:
- Heaviness and discomfort
- Urinary leakage or retention
- Frequent Urinary Tract Infections
- Backaches
- Abnormal bowel movements
In more severe cases, the prolapse may be seen partially or completely protruding out of the vagina.
You might have to get a vaginal hysterectomy
Vaginal hysterectomy is usually recommended for fit and mobile patients with severe prolapse. They are also recommended for those in which conservative treatments with physiotherapy (Kegels exercise) and vaginal pessaries have failed to relieve their symptoms.
In this case, the uterus is commonly removed vaginally and any loose vaginal skin is excised. The weakened and lax vaginal supports are then strengthened with strategically placed sutures.
4. Gynaecological Cancers
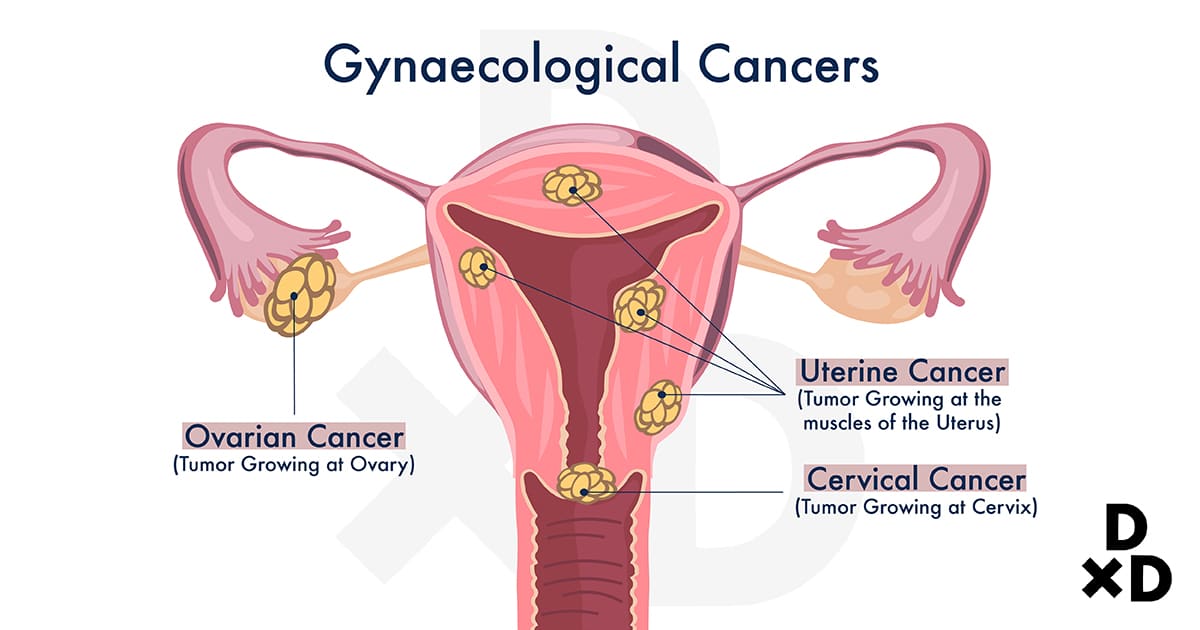
This refers to Ovarian, Uterine, and Cervical Cancers. Depending on the stage of the cancers, the gynaecologist may perform either a total hysterectomy (removal of the body of the uterus and cervix) or a radical hysterectomy (removal of the uterus, cervix, the upper part of the vagina, and nearby tissues).
Chemotherapy and/or radiotherapy may follow after the surgery depending on the stage and nature of the cancer. Read along to find out more about the different types of hysterectomy!
Related: The Ultimate Guide to Gynaecological Conditions in Singapore (2021)
What are the types of Hysterectomies?
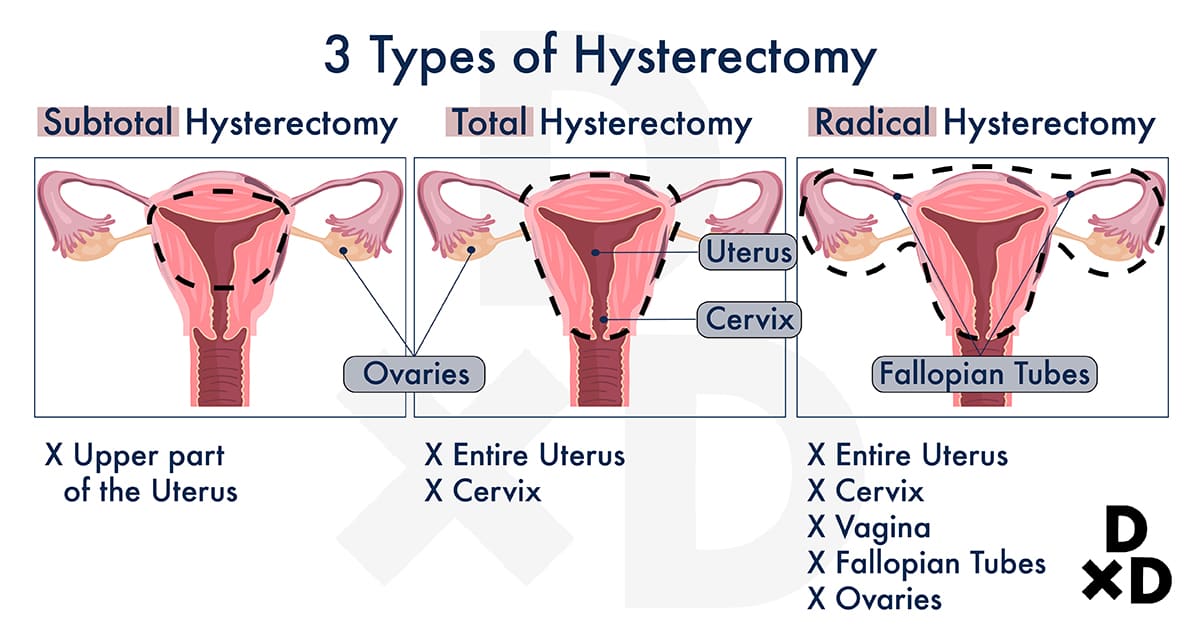
A total hysterectomy refers to the removal of the uterus and cervix (neck of the uterus) together while a subtotal hysterectomy removes only the uterus leaving the cervix behind. Occasionally, a hysterectomy may be combined with the removal of the fallopian tubes (salpingectomy) and the ovaries (oophorectomy).
Also read: Dealing With Cervical Cancer: A Women's Gynaecological Cancer Awareness Campaign
There are 3 Methods of Hysterectomy
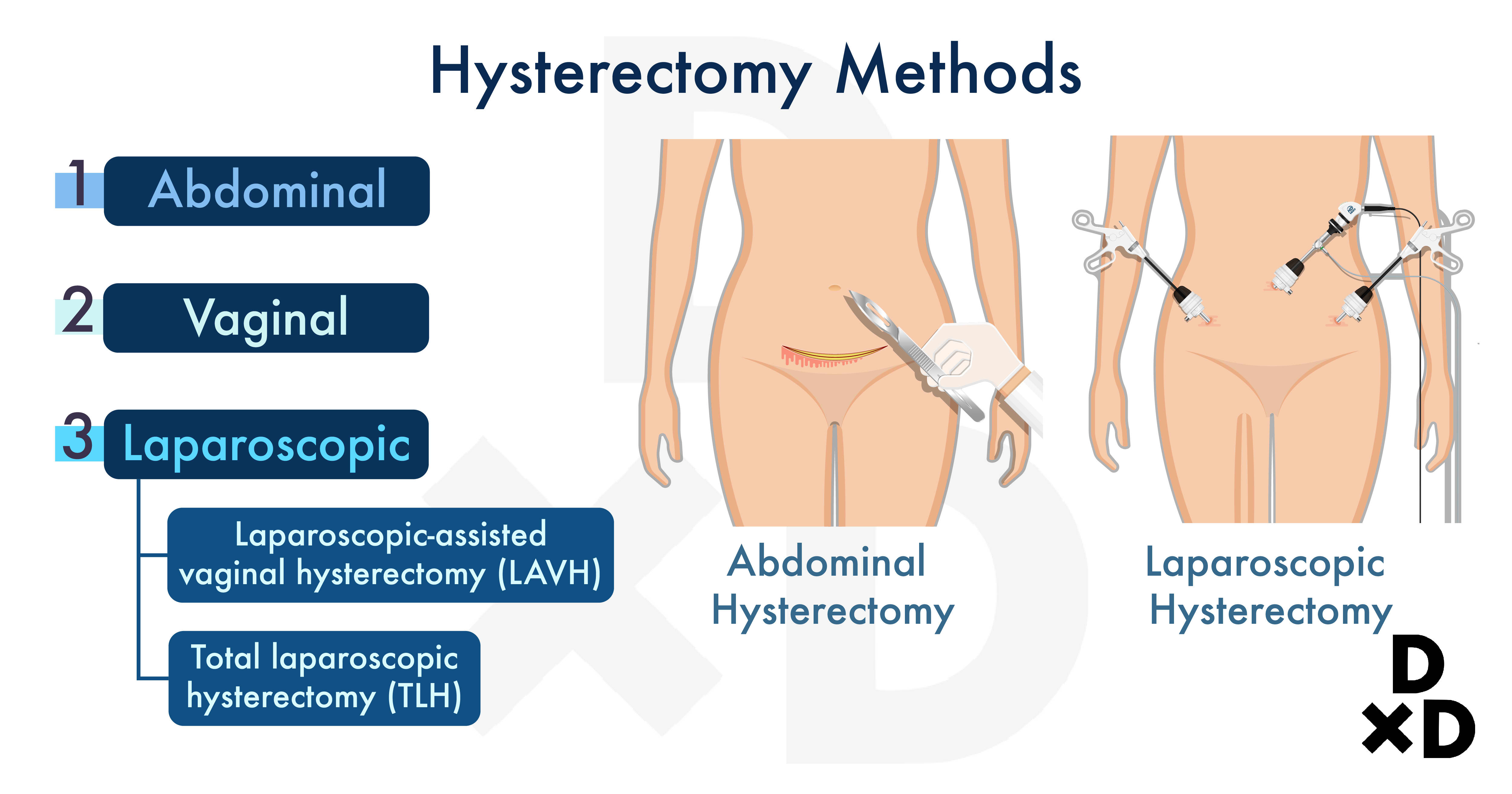
They can be performed via an open abdominal incision (laparotomy), tiny abdominal key-hole incisions (laparoscopy) or vaginally [8].
Abdominal Hysterectomy (laparotomy)
This is the most common method used if the patient has endometriosis or other pelvic diseases. Both total and subtotal hysterectomy are done through this method. Compared with all other type and methods, total abnormal hysterectomy is the most common.
The recovery time differs between patients. With adequate analgesia, the procedure should be relatively pain-free.
Related: When is a total abdominal hysterectomy salpingo-oophorectomy surgery recommended?
Vaginal Hysterectomy
There is no abdominal scar but it might not be suitable for everyone. This method is commonly used to treat uterine prolapse.
Note that the type and method can only be determined after a thorough consultation with your doctor! It might be different for everyone.
Laparoscopic Hysterectomy
The procedure itself may take longer as compared to other methods but it is known to have a rapid recovery time.
There are 2 sub-categories:
- Laparoscopic-assisted vaginal hysterectomy (LAVH)
- Total laparoscopic hysterectomy (TLH)
What are the pros and cons of each method?
Method
Pros
Cons
Abdominal [9]
Suitable for those with an enlarged uterus
Involves an abdominal scar
Longer recovery time
Vaginal [10]
Less invasive
Faster recovery as compared to abdominal
No external incision and thus no visible scarring
Cannot be performed for cancer cases
Difficult to perform if there are pelvic adhesions
Laparoscopic-assisted vaginal (LAVH) [10]
Recovery time for LAVH is usually significantly less than an abdominal hysterectomy
Uterine attachments (ligaments) and vessels can be ligated laparoscopically for cases in which there is no uterine descent. The uterus can then be removed vaginally, especially for women who have not had children.
More costly to perform
More surgical training required for the gynaecologist
Potentially longer operating time compared to other methods
Total laparoscopic [9]
- Small or non-visible surgical scars on the tummy
- Reduced pain after surgery
- Less bowel function disturbances
- Shorter recovery time
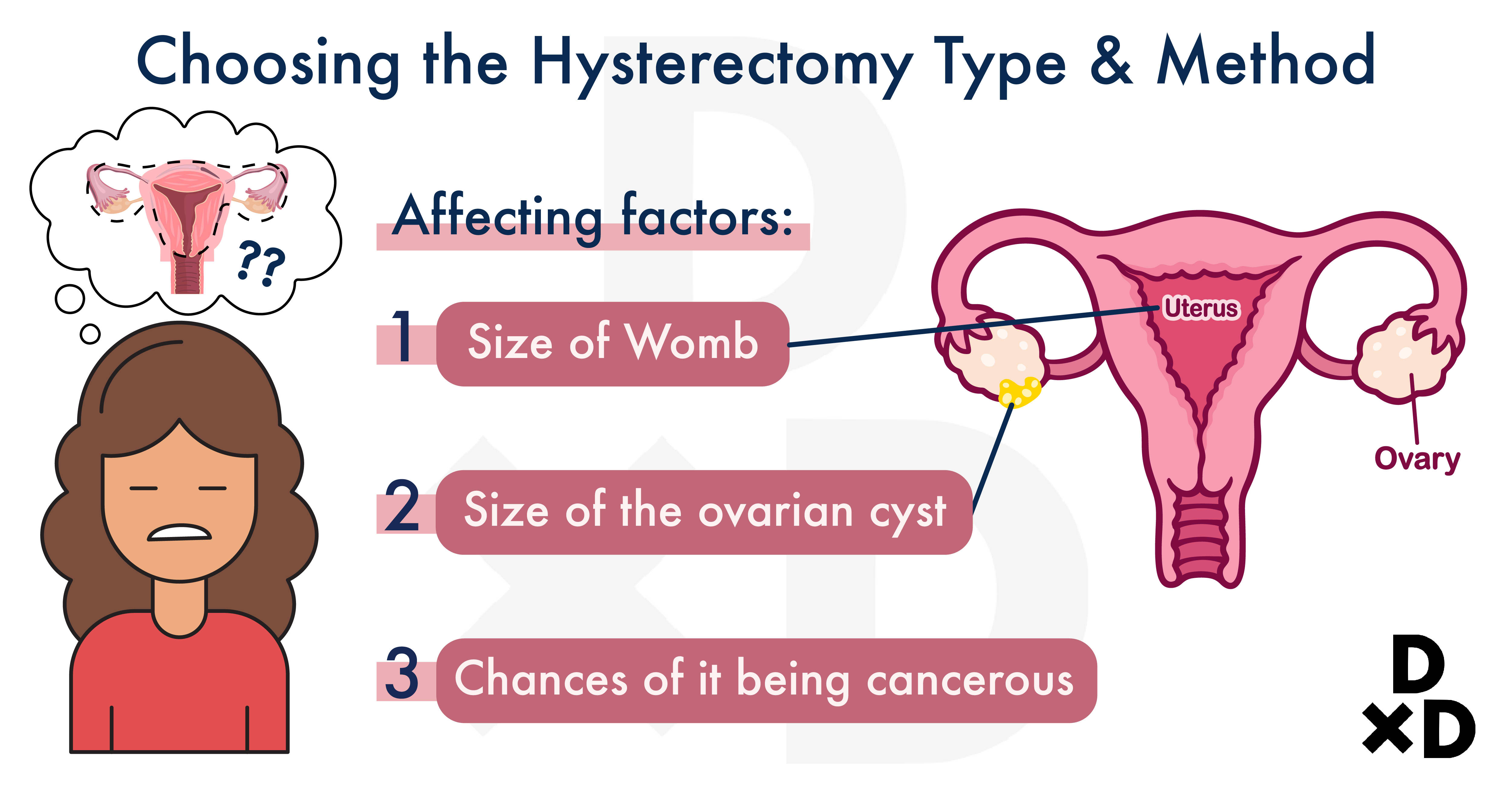
What are the factors to consider when choosing which procedure to undergo?
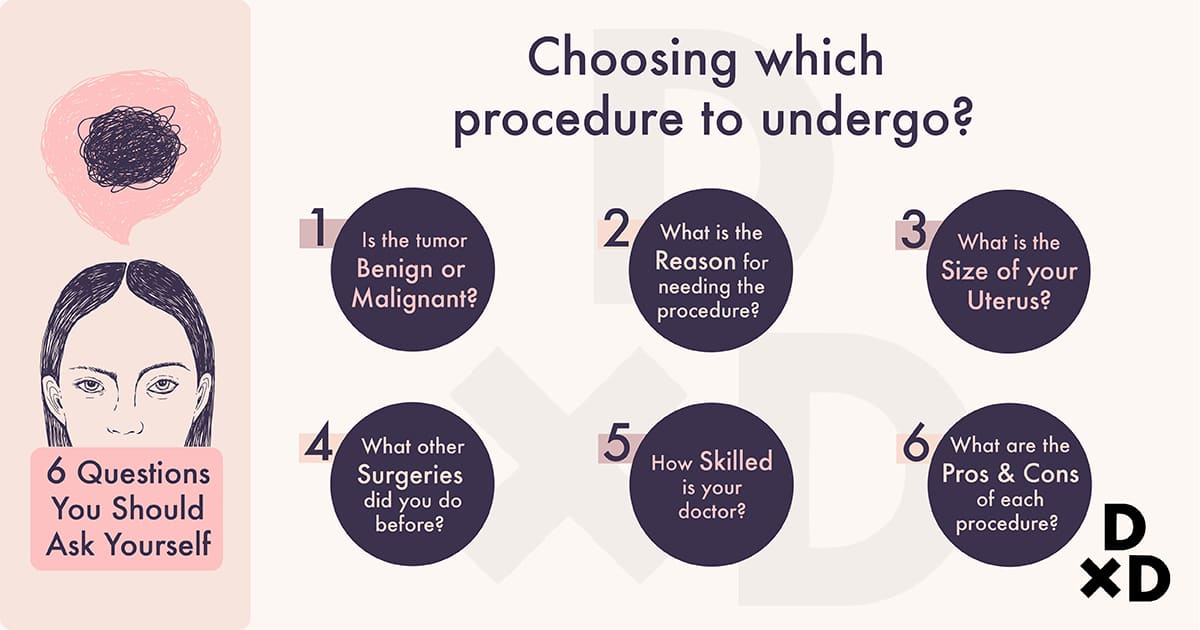
Women who opt for hysterectomy are usually those who have been unsuccessful with other medical treatments. An important note is that you will not be able to conceive after the surgery.
The type of hysterectomy (simple, subtotal, radical) and the method (abdominal, vaginal, laparoscopic) depends on many factors like:
- Indication for surgery (benign or malignant)
- Pathology involved (fibroids, endometriosis, prolapse, cancer)
- Size of the uterus
- Previous surgeries
- Skills of the gynaecologist
This is why a detailed consultation and an informed consent must be obtained before proceeding with the hysterectomy. In whatever case, do consult your gynaecologist before proceeding with any procedure!
What are the side effects from getting a hysterectomy?
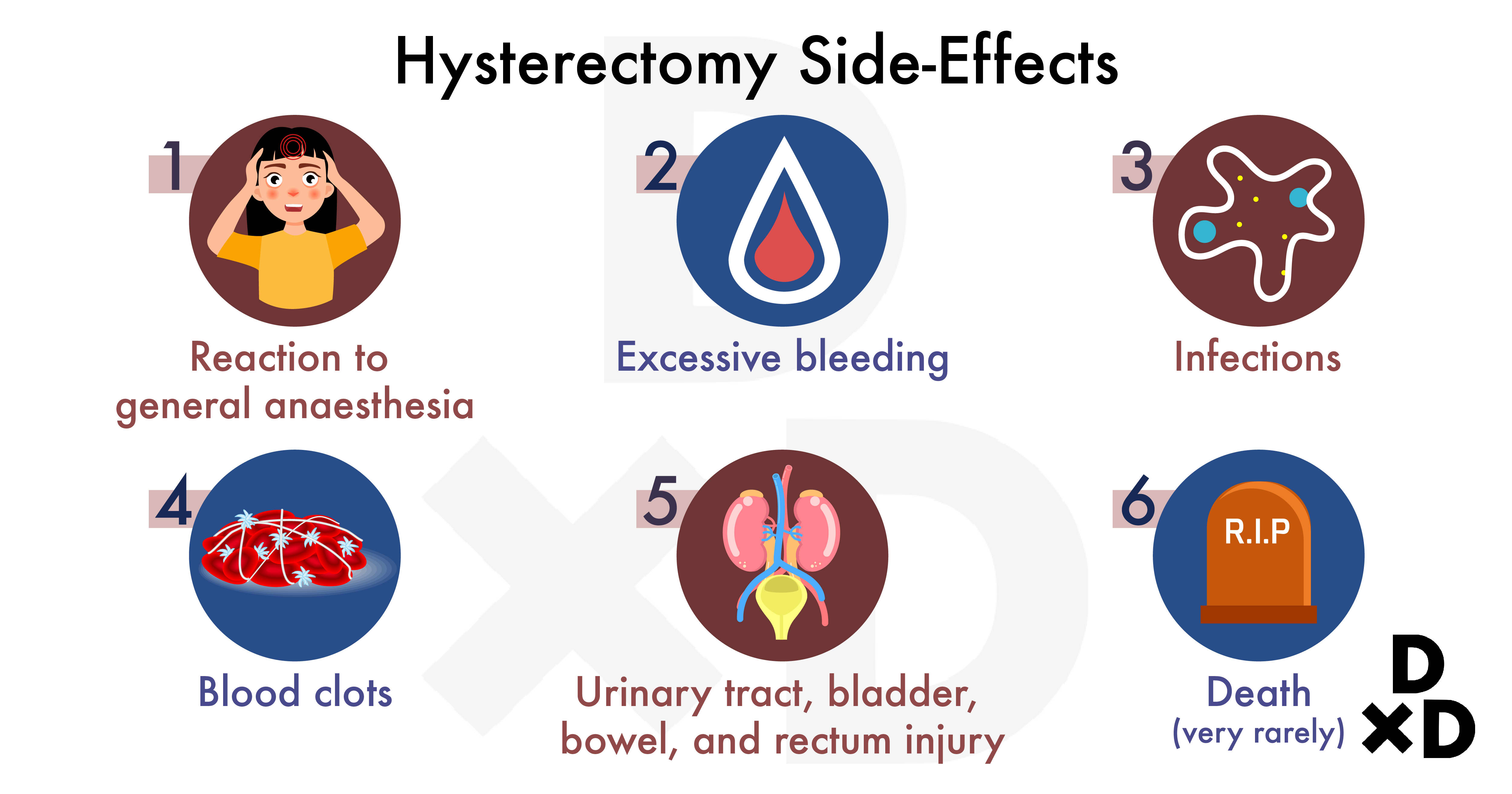
Hysterectomies tend to be safe. But like any major surgery, they are associated with several potential complications: [8]
- Reaction to general anaesthesia
- Excessive bleeding
- Infections
- Blood clots
- Urinary tract, bladder, bowel, and rectum injury
- Very rarely, death
For all these potential risks there are precautions taken to minimise their occurrence. At the end of the day, women should always know why they agree to undergo a hysterectomy. The general principle is that they should not go for any surgery unless they are aware of the benefits and risks, and are convinced of the need for it. I would always recommend that you explore all non-surgical options first!
What should I expect after a Hysterectomy?
There will be a few manageable changes after the procedure. It is best to be familiar with them before you decide on taking the surgery!
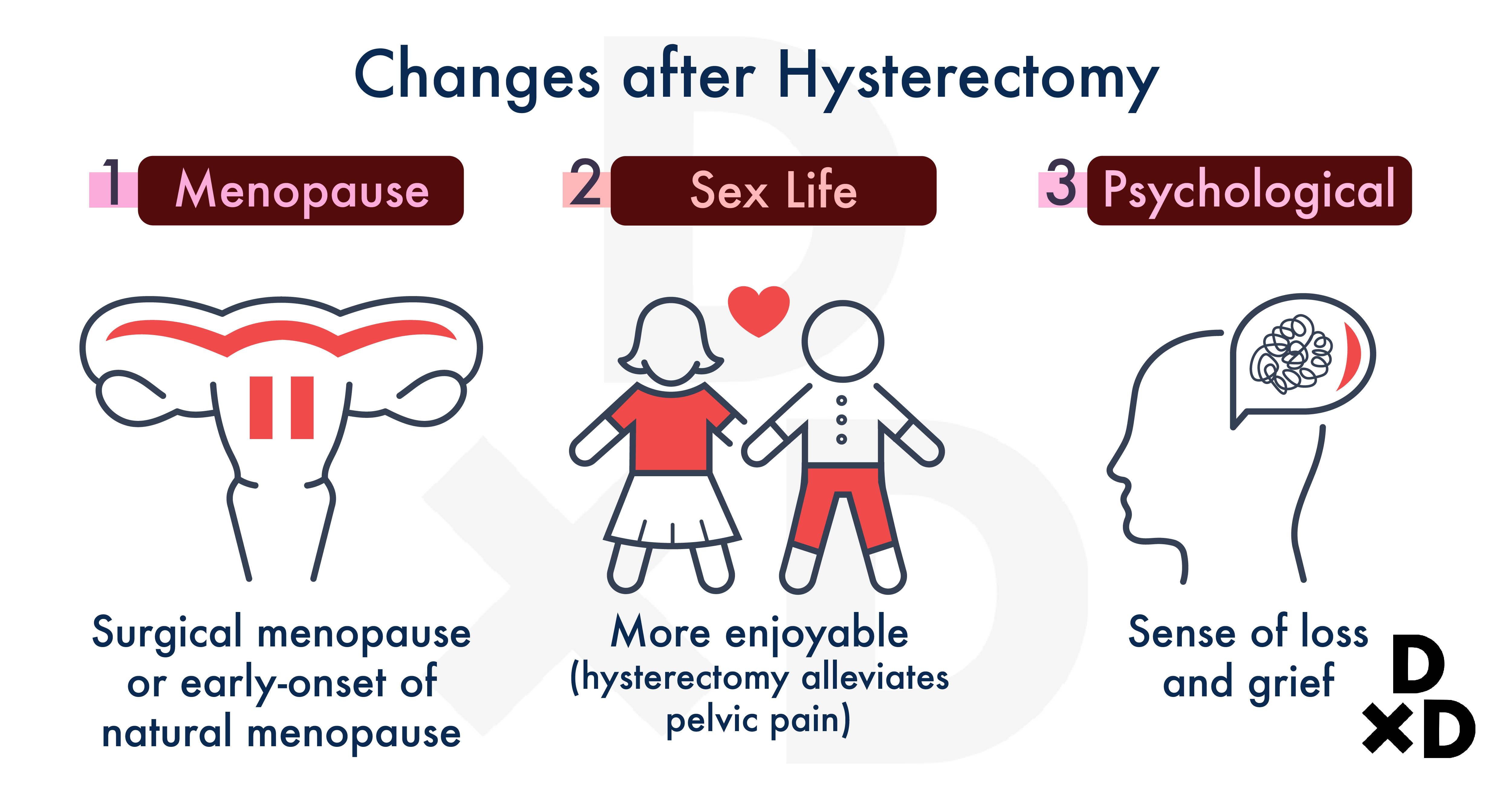
1. Menopause
After a hysterectomy, your menstrual period will stop and you will not be able to conceive.
If your ovaries are removed along with hysterectomy, menopause will start right after the procedure. This is called surgical menopause. Most women will experience menopause symptoms within a few days after the procedure.
If your ovaries are not removed, there is still a risk of premature menopause [11]. However, this is uncommon! If the ovaries were not damaged and are functioning well, there should be no complications.
2. Change in sex life
It is recommended that you wait 4-6 weeks after the surgery before having sex. This might differ so it is always best to check with your doctor.
Though uncommon, some people have noted lower sexual desire. In most cases, however, there should be almost no changes if you have had a good sex life before the procedure. In cases where the hysterectomy is done to treat pelvic pain, sex might even be more enjoyable [11].
As mentioned before, women will not be able to conceive after a hysterectomy. As such, you would no longer need contraception.
3. Psychological changes
Some women might have no other option but to get a hysterectomy. This is especially the case for those with gynaecologic cancers.
For women of child-bearing age, this may come with grief over the loss of fertility. Changes in your hormonal level may also temporarily affect your emotions. This is not surprising as researches have documented a link between changing hormone levels and depression in women [12].
Before getting a hysterectomy, make sure you research through and consult an experienced doctor. It is always best to understand and acknowledge the benefits and risks of a certain procedure before getting them.
If you feel depressed or have any sense of loss after a hysterectomy, consult your doctor immediately!
Also read: The Best Tips From A Singaporean Psychiatrist On How To Take Care Of Your Mental Health
Hysterectomy is Linked with Coronary Artery Disease (CAD)
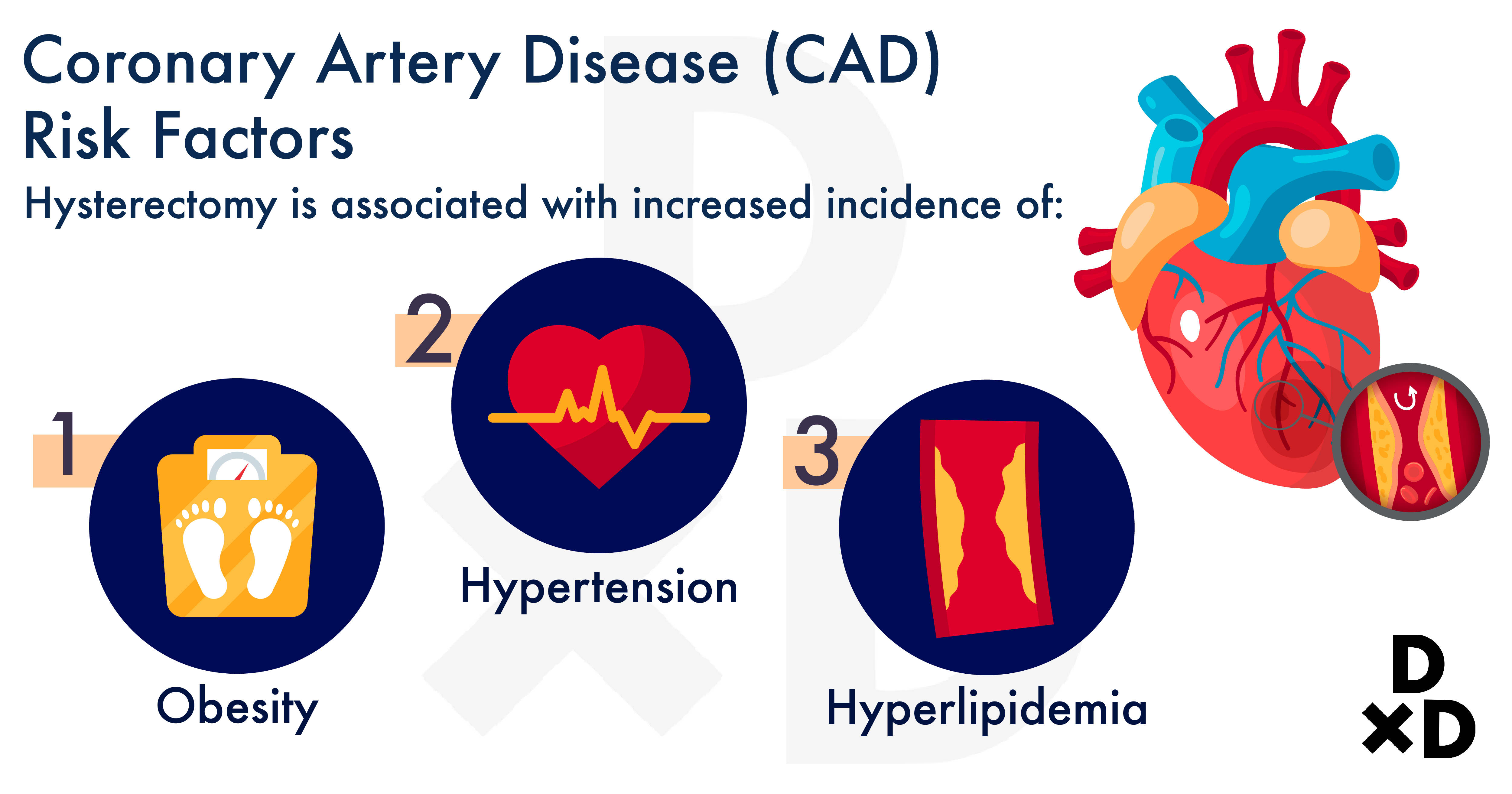
Various researches have shown that hysterectomy is associated with an increased incidence of various cardiovascular risk factors such as:
- Obesity
- Hypertension
- Hyperlipidemia (too much cholesterol and other fats)
Read more: The Tell-All Guide to Cardiovascular Risk Reduction in Singapore (2021)
This association is found in women of all ages. However, CAD risks are much more elevated in those aged 50-79 years old.
On top of that, the same study found an association between hysterectomy and a higher risk of stroke. This risk is more elevated in women under 30 years old [13].
Related: Can coronary artery disease to be treated with only medication and exercise?
Chronic Post-Hysterectomy Pain (CPHP) is the Most Common Complication
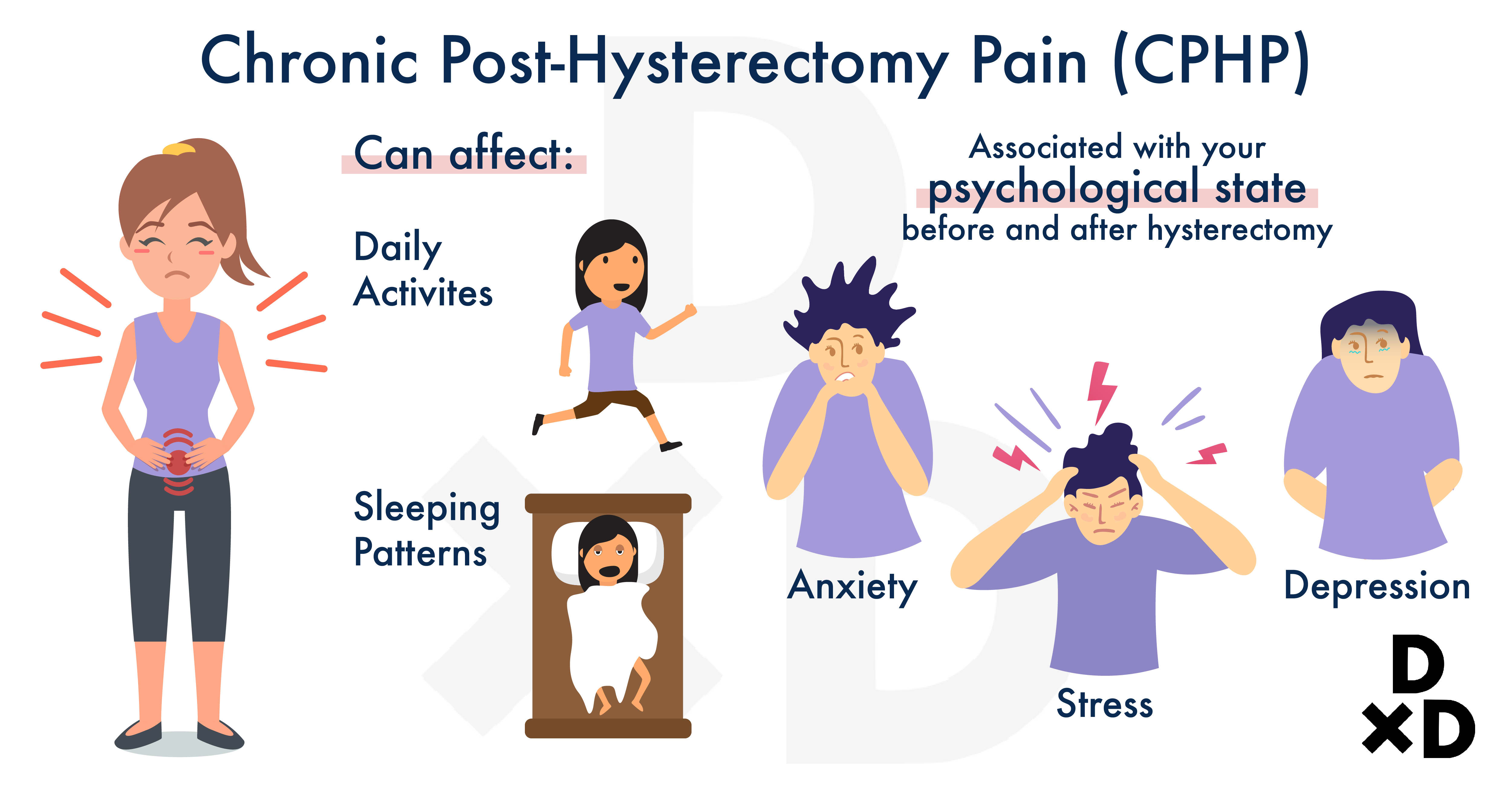
A cohort study found that CPHP is present 4-6 months after the procedure. They are problematic as they may interfere with your daily activities and sleep patterns. That said, most cases of CPHP resolves with time.
The condition is found to be associated with acute pain during and right after the procedure. To prevent CPHP, it is best to get an aggressive treatment for acute pain immediately after the hysterectomy itself [14].
If you experience any pain after the surgery, do consult your doctor immediately! It is best to treat any discomfort as early as possible.
CPHP is also associated with the psychological state of women before and after the procedure. Research found that there is a higher risk of developing CPHP in women with: [15]
- Stress and anxiety BEFORE the hysterectomy
- Depression, anxiety, or a great sense of loss AFTER the hysterectomy
As previously mentioned, it is best to understand all the risks of the procedure. If you feel stressed, depressed, or stressed, do consult your doctor!
Related: How can I get help if I have anxiety issues in Singapore?
How is Hysterectomy conducted with Robotic Surgery?
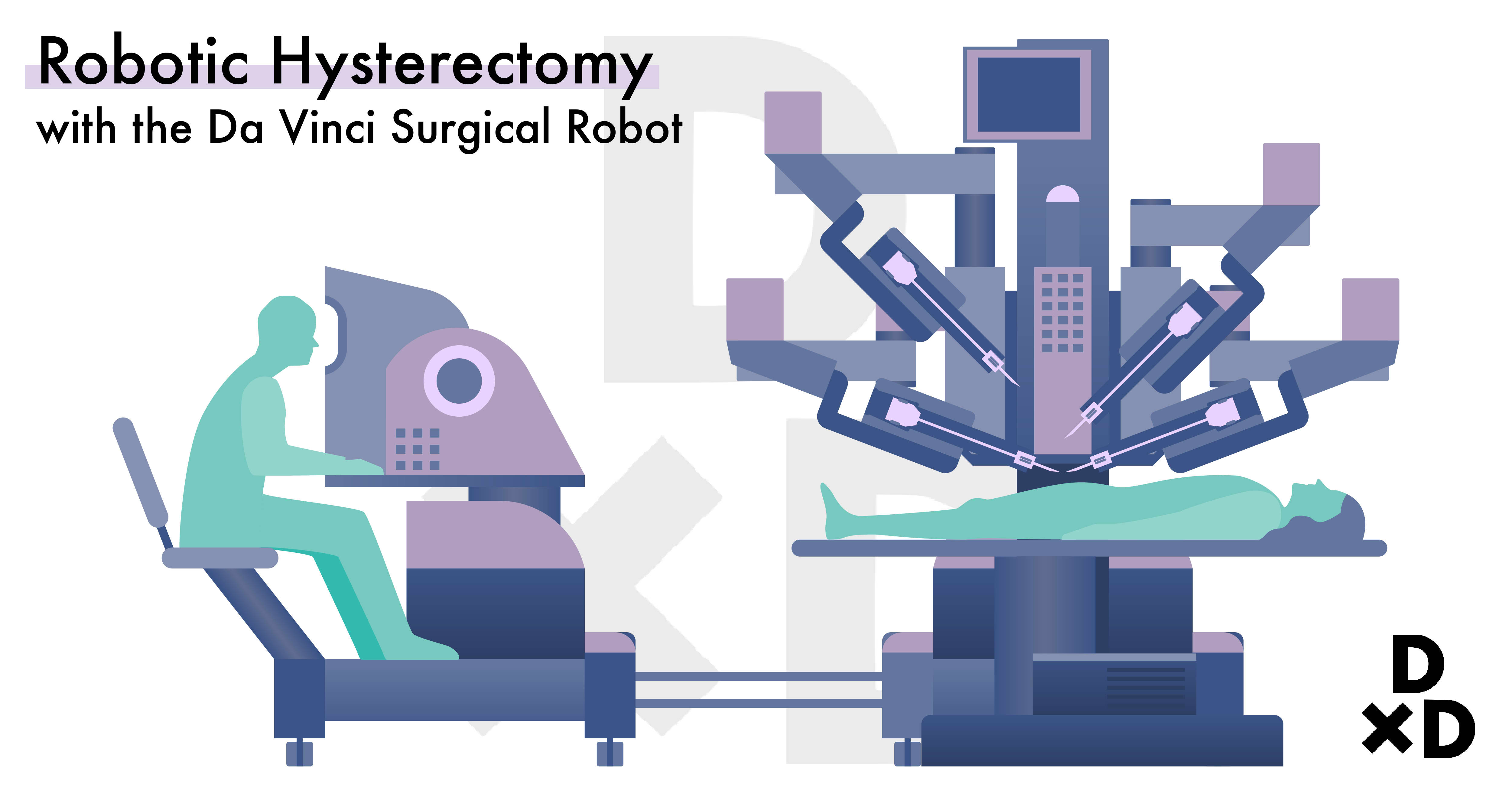
Surgical treatments with the da Vinci surgical robot is available at various major hospitals in Singapore. For gynaecology, however, its use is still very limited. This is because:
- A higher cost involved in operating the robot
- The procedure may take a longer time to complete
- Patients are exposed to anaesthesia for a longer time, increasing the risks of adverse reactions
- Similar recovery time as other methods
What procedure is for me?
There are different types and methods. As previously mentioned, vaginal hysterectomy is commonly used to treat uterine prolapse.
For other diseases, whether the hysterectomy is performed as robotic surgery, an open procedure (laparotomy) or keyhole (laparoscopic) depends on:
- Size of the womb
- Size of the ovarian cyst
- Chances of it being cancerous
You should discuss and learn more about all the methods with an experienced doctor before giving consent!
How much does a Hysterectomy cost?

The surgeon's fee alone could range anywhere between S$9,000 - S$17,000. This price may vary depending on:
- Type of hysterectomy
- Method of hysterectomy
- The complexity of the condition
- Whether the surgery is for benign or cancerous conditions
- Experience of gynaecologist
- Public or Private hospital
Is a Hysterectomy Medisave-Claimable?

A hysterectomy for most cancerous or non-cancerous conditions is Medisave-claimable. The amount depends on your condition and the diagnosis.
For the hysterectomy surgery alone, you can claim:
Amount Claimable
Simple open hysterectomies
$2150
Laparoscopic or robotic
$3150
Complicated endometriosis;
Broad ligament tumour;
Gynaecological cancers
$3950
You can check with your doctor for more information.
Importance of Screening
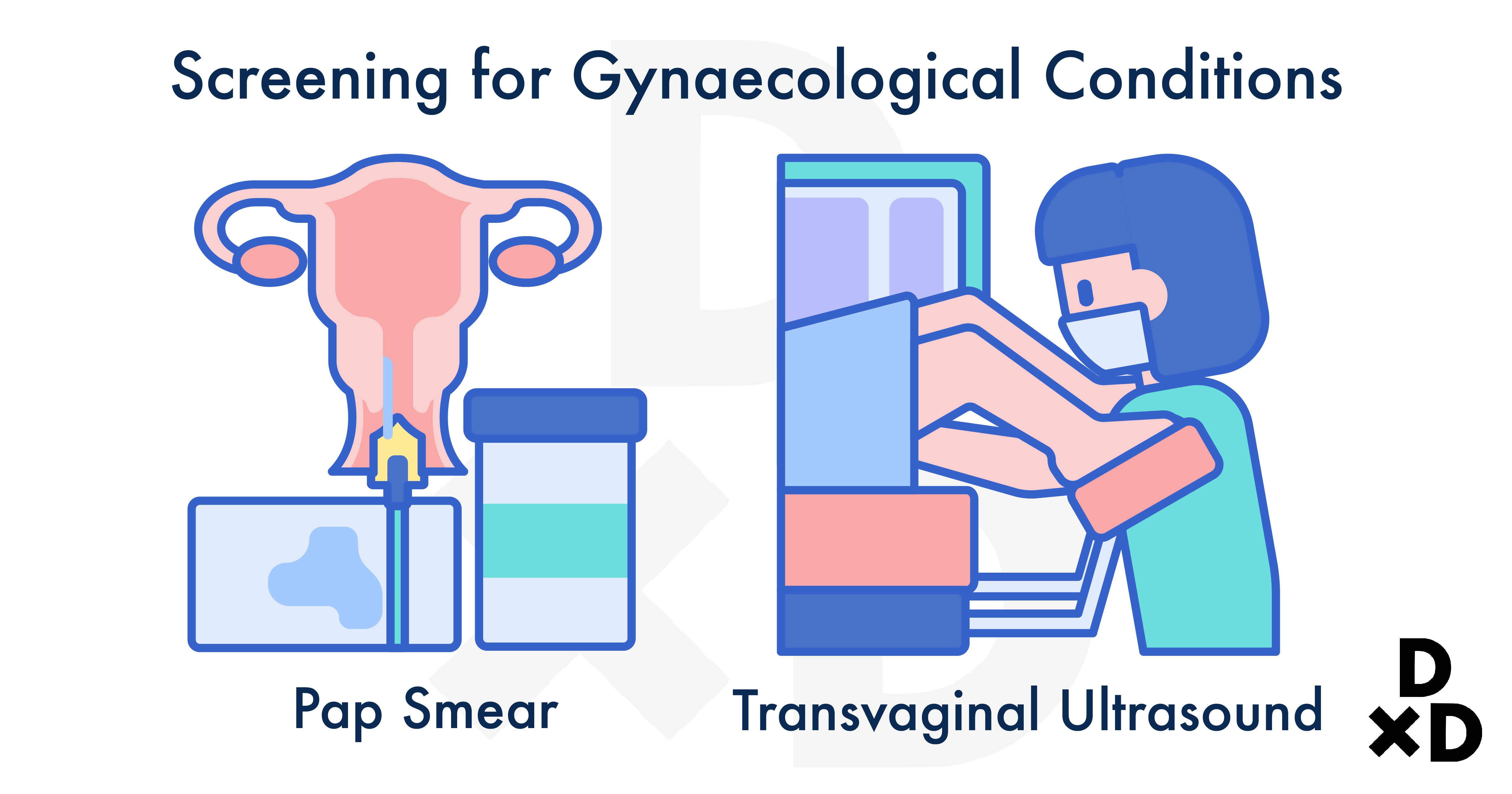
Endometrial or uterine cancer is the fourth most common cancer in Singaporean women. The number of cases is also expected to increase [16]. Fortunately, most cases can be detected early as there are physical symptoms such as abnormal menstrual bleeding.
At times, other gynaecological cancers may not present such symptoms in the early stages. I would always recommend that you get a routine Pap test and pelvic exam with transvaginal ultrasound to screen for possible cancers.
Hysterectomies play an important role in treating various gynaecological conditions. It is also one of the most common gynaecological procedures! They have proven to be an effective cure for most gynaecological cancers and benign gynaecological conditions.
That said, the first step is always consultation and medical check-up. If you ever feel any discomfort around your pelvic area or see some of the symptoms previously mentioned in the article, do consult your doctor! It is always best to diagnose a condition early so that various treatments can effectively help you feel better.
I wrote this article to give you an extensive guide on hysterectomy. I understand that the different information available online about the different hysterectomy methods in Singapore might be confusing. I sincerely hope that this helps your research!
In any case, always consult an experienced doctor to explore non-surgical options before choosing to get a hysterectomy. When it is deemed necessary, also consult them to see which type and method are most suitable for you.
Dr Christopher Ng is a gynaecologist with GynaeMD Women's & Rejuvenation Clinic. He is accredited to perform Level 3 laparoscopic (minimally invasive) surgeries on top of general gynaecology surgeries. He also performs surgery for urinary incontinence and uterovaginal prolapse.
Read more of Dr Christopher Ng's QnA here.
Would you like to ask any related health questions?
You can Ask A Doctor right away, or request for treatment quotes from doctors.